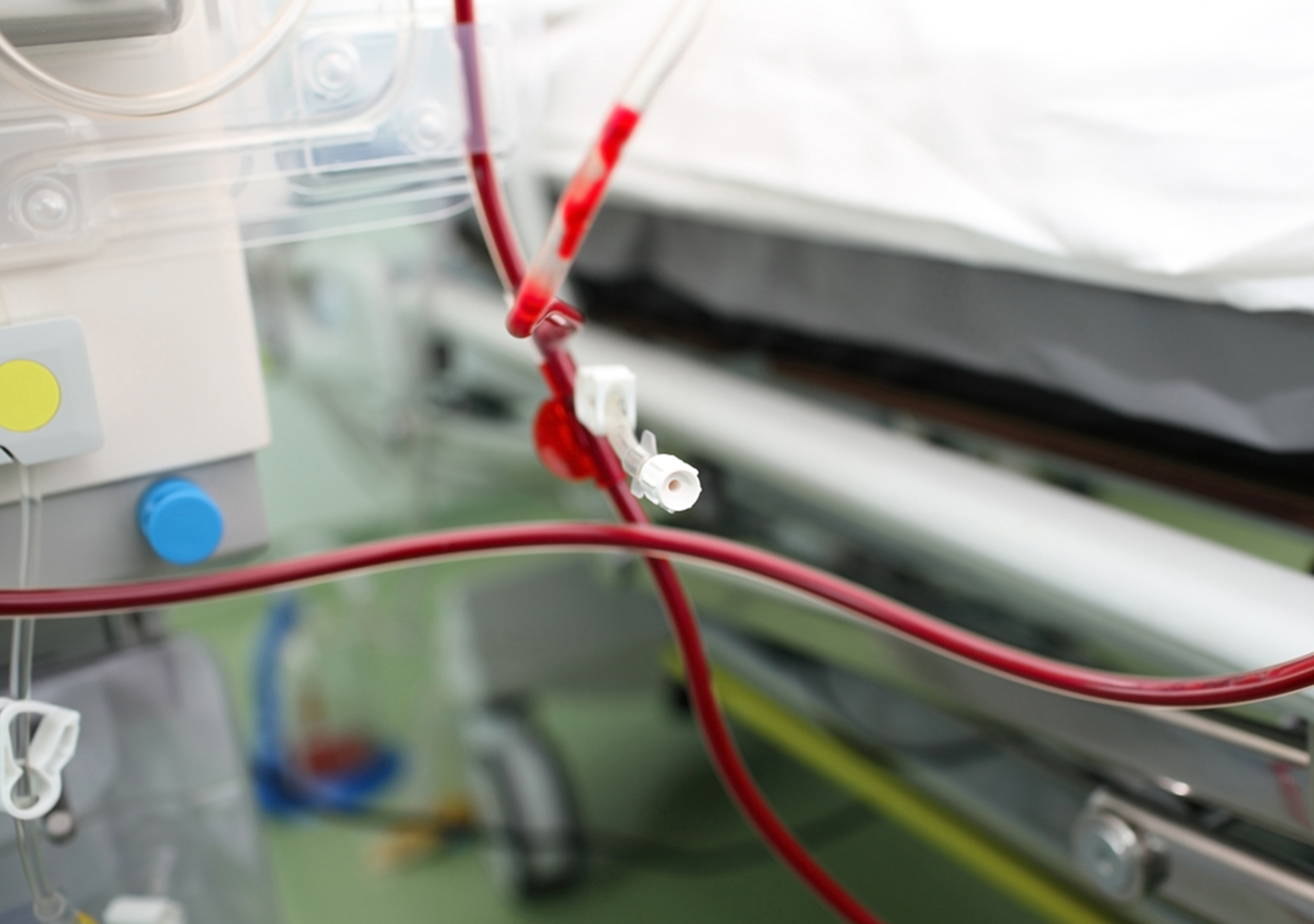
The risks and complications of blood transfusion are well documented. One technique commonly used to help reduce the need for bank blood is autotransfusion, also referred to as intraoperative autotransfusion (IAT) or autologous blood transfusion. IAT is a method of collecting the patient’s blood lost during surgery, processing it, and returning it to the patient. This can significantly reduce, or even eliminate the need for blood transfusions, which in turn reduces complications and the cost of care.
Al Stammers, MSA, CCP, SpecialtyCare’s Director of Clinical Quality and Outcomes Research, recently looked at our IAT data as documented in SCOPE, the SpecialtyCare Operative Procedural Registry®. SCOPE is the largest registry of perfusion-related data in the U.S., and is used for quality improvement and to conduct original research.
 Our analysis found that SpecialtyCare associates using IAT during open heart surgery processed and returned over 10 million cc of red blood cells (RBC) during the first eight months of 2017. This is equivalent to over 41,000 units of blood. Looking at this on an annualized basis, we estimate that over 60,000 units of our patients’ blood was returned to them, thus greatly reducing the need for bank blood transfusions.
Our analysis found that SpecialtyCare associates using IAT during open heart surgery processed and returned over 10 million cc of red blood cells (RBC) during the first eight months of 2017. This is equivalent to over 41,000 units of blood. Looking at this on an annualized basis, we estimate that over 60,000 units of our patients’ blood was returned to them, thus greatly reducing the need for bank blood transfusions.
We are currently experiencing a blood shortage across the nation. Increased demand from a growing number of complex therapies, such as cancer treatments and organ transplants, has the increased need for blood far outpacing the number of donations. Through the use of IAT, we are able to help lessen this demand.
The benefit to our patients can be significant. Reducing blood transfusions reduces the complications associated with transfusion, which include allergic reaction, infection, renal failure, heart attack, stroke, or even death. Fewer complications result in shorter ICU stays, less ventilator time, and overall shorter hospital stays.
IAT also reduces cost. Most hospitals purchase their blood from either non-profit or private blood centers. On average, the acquisition cost for a single unit of RBCs is $750. When you add in the costs of processing, handling, and storage, the cost for transfusing one unit of blood approaches $1,200. And this does not include the costs of complications from the transfusion, which are estimated to be around $1,480 per unit.
Through processing and returning 60,000 units of the patients’ own blood, we can potentially save our hospital partners $45 million in acquisition costs alone. Add in processing and the cost of complications associated with transfusion, and the savings approach $90 million per year.
This intraoperative autotransfusion analysis is just one example of the many ways we use SCOPE to provide benchmarks for standards of care that our customers rely on to measure and improve their performance, both internally, and against their peers. The data, combined with clinical expertise, results in quality outcomes, clinical excellence, innovation, and cost containment for our patients and hospital partners.
LEARN MORE ABOUT PERFUSION
LEARN MORE ABOUT AUTOTRANSFUSION
###
Contact us at [email protected] to learn how you can pair expertise in IAT, patient blood management, and other programs with national benchmarking and clinical variation analysis to find opportunities to improve patient care and reduce costs for your organization.


Comments are closed.