ATS Week ’24 with Kimberly Sharp, ATS Clinical Manager
As Autotransfusion Week 2024 unfolds, we find ourselves immersed in a celebration of the extraordinary individuals...Cesar Jaime
Paige B. and Jasmine M. Posing infront of machine – blue caps @ Novato Surgery center…
Revolutionizing Cancer Treatment: The Rise of HIPEC and Perfusion Therapy
Cancer incidence is on the rise, and the American Cancer Society forecasts that there will be...ECMO Success Story: Baby Theo Recovers from Severe Meconium Aspiration Syndrome
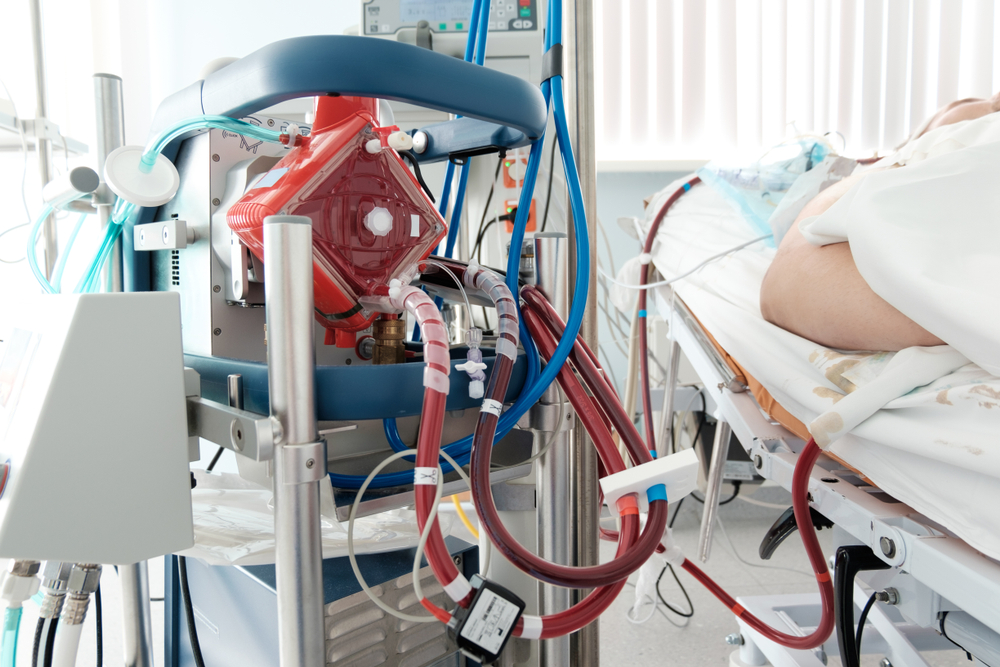
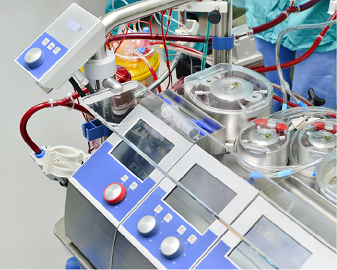
ECMO therapy can offer life-saving intervention for those suffering from a respiratory crisis. The use of...Medical Missions: SpecialtyCare Team Members Serve in Honduras and Barbados
This year, some of our team members at SpecialtyCare have been involved in trips where they...“Far More Fulfilling Than I’ve Ever Thought About”: Dionna Ellis, Clinical MI Specialist IV, on the Rewards of Being a Clinical Specialist
Ask any professional: Beyond simply making a living, doing work that is truly rewarding is the...“I Get to Make a Difference”: Landon Jackson, Clinical MI Specialist III, on Passion and Fulfillment
Though they share similarities, every surgical case is different: every person, their health history, their background,...“It’s a Very Rewarding Field”: Austin McFadden, Clinical MI Specialist I, on Teamwork and Success
At SpecialtyCare, we’re dedicated to your success. But, you don’t have to simply take our word...“The Day-to-Day Is Never the Same”: Jean-Imani Phipps, Clinical MI Specialist III, on the Value of Variety
Monotony can put a damper on any kind of job. The healthcare industry has its patterns...September Perfusion Webinar: Great Documentation, Not Something to Bypass!
Join us in discussing clinical documentation with Debra Weinrich, LLP. Learning Objectives include: -Identify some common...Perfusion Webinar Series: “May 6, 1953, Operative Report: Closure of a large interatrial septal defect…easily closed”
Join Mark Kurusz as he shares an appreciation of history in the context of current CPB...Neurosurgery Awareness Month 2023
August is Neurosurgery Awareness Month, a time to recognize the impact of traumatic brain injuries, appreciate...The Demand for ECMO Specialists Is Rising. Here Are the Benefits of Becoming One.
ECMO therapy has increased significantly over the past two decades. Nearly half the ECMO cases recorded...What Is CAP Accreditation, and How Does It Apply to Your Autotransfusion Services?
The College of American Pathologists (CAP) has an accreditation program for laboratories to ensure quality standards...Sam Weinstein, MD, Named to Nashville Health Care Council’s Board of Directors
SpecialtyCare Chief Executive Officer Sam Weinstein, MD, has been appointed to the Nashville Health Care Council’s...Neurological Health Takes the Spotlight for World Brain Day
July 22, 2023, is World Brain Day, and the theme is Brain Health and Disability. But,...Are Your Nurses Prepared to Manage Your Autotransfusion?
Autotransfusion is safer and more efficient than traditional donor transfusions, eliminating intermediate processes and costs while...Surgical Neurophysiologist Job Opening in Jacksonville, FL
Jacksonville, Florida, a beachside city home to nearly one million people, is located on the Atlantic...Surgical Neurophysiologist Job Opening in Charlotte, NC
Charlotte, North Carolina, is a thriving metropolis located just a few hours away from both the...Why Choose SpecialtyCare for Your IONM Career?
SpecialtyCare is an excellent choice for starting or building your IONM career. As the demand for...Why More Surgeons Are Using Autotransfusion at Ambulatory Surgery Centers
More spinal and hip surgeries are being conducted at ASCs, likely because rates of infection are...The Value of Mentorship in IONM: An Interview with Clinical Instructor Devin Cross
Devin J Cross MS, CNIM, Sr SN III, Clinical Instructor Mentorship is a key vehicle for...Mentorship Spotlight: “Having a Mentor like Kaytie Will Set You Up for Success in the IONM Field”
In the medical field, there are countless skills you can’t learn from textbooks or labs. They...Benefits of Being a Mentor to Up-and-Coming Medical Professionals
Have you ever considered being a mentor to younger or less experienced medical professionals? The truth...5 Advantages of Having a Mentor in the Medical Field
Courses, training, and practice are critical to building knowledge and skills in medicine. But, mentorship provides...SpecialtyCare Team in Minneapolis Raises Over $3K for Special Olympics By Taking the Polar Plunge
At SpecialtyCare, it’s not just our high quality services that set us apart — it’s our...Day in the Life: ATS Edition with Abigail Pamenter
We greatly appreciate and value all of our SpecialtyCare ATS employees. We’re highlighting clinician Abigail Pamenter,...The Use of Transcranial Doppler for Detecting Subarachnoid Hemorrhage
Transcranial Doppler (TCD) is a safe, noninvasive method for identifying and tracking the presence of emboli....Day in the Life: ATS Edition with Melody Davis
We greatly appreciate and value all of our SpecialtyCare ATS employees. We’re highlighting Clinical Manager Melody...Transcranial Doppler and Emboli Monitoring
Emboli can cause a range of disrupting and even life-threatening conditions, but their presence is not...How Your Hospital Saves Millions of Dollars Per Year by Improving Sterile Processing Quality
With many hospitals operating in the red, it would seem like no financial losses are going...Day in the Life: ATS Edition with Yessenia Avila-Newberry
We greatly appreciate and value all of our SpecialtyCare ATS employees. We’re highlighting Yessenia Avila-Newberry, Clin,...Day in the Life: ATS Edition with Amanda Hill
We greatly appreciate and value all of our SpecialtyCare ATS employees. We’re highlighting Amanda Hill, Clinical...SpecialtyCare Attends AMSECT 2023 to Engage in the Latest Regarding Perfusion & ECMO
SpecialtyCare attended AMSECT 2023 from March 22-24, 2023, in Orlando, FL, to engage in the latest...ECMO Success Story: Florida Asthma Patient Recovers from Life-Threatening Attack
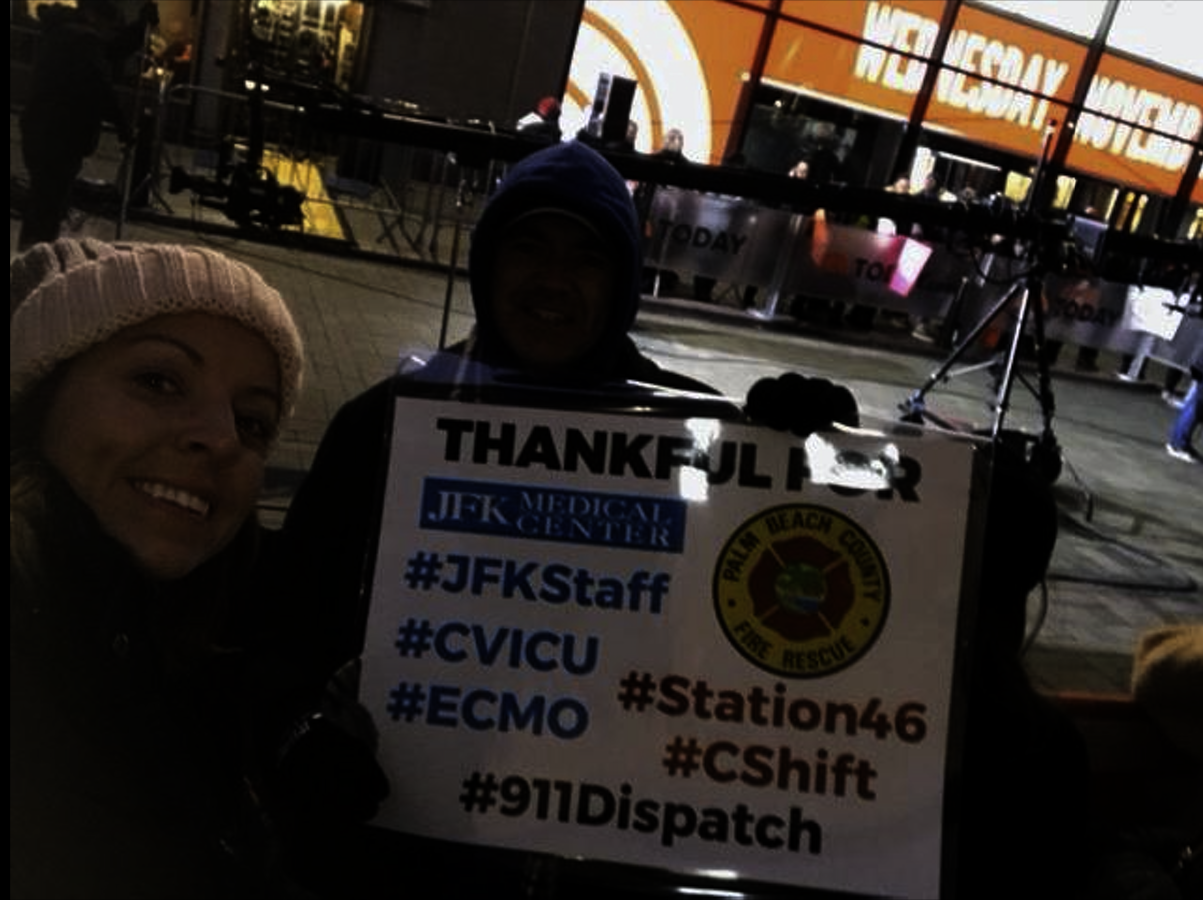
As the largest provider of ECMO in the US, SpecialtyCare offers training and places ECMO specialists...Benefits of Utilizing Transcranial Doppler (TCD) Services at Your Hospital
Benefits of Utilizing Transcranial Doppler (TCD) Services at Your Hospital As today’s OR innovations enhance patients’...When Santa Claus Provides Transcranial Doppler Services at Your Hospital
At the hospital leadership level, patient care is often spoken of in terms of improving outcomes,...SpecialtyCare Provides Services at 120 of the 250 Best Hospitals in the US
We would like to congratulate all the hospitals that made Heathgrades’ list of the top 250...February Is American Heart Month: How Can We Make Heart Surgery Safer?
According to the Centers for Disease Control (CDC), 1 in 5 deaths in the US could...How Tray Optimization Can Help Hospitals Cut Costs in 2023
It’s no secret: Hospitals are still reeling from the financial impact of the COVID-19 pandemic. The...Surgical Neurophysiologist Job Opening in San Antonio, TX
By joining SpecialtyCare, you become a very important part of the surgical and patient care teams,...We’re Hiring for a Surgical Neurophysiologist in Seattle, WA
By joining SpecialtyCare, you become a very important part of the surgical and patient care teams,...Surgical Neurophysiologist Job Openings in Kansas: Wichita and Kansas City
By joining SpecialtyCare, you become a very important part of the surgical and patient care teams,...We’re Hiring for an EEG Tech in St. Cloud, MN!
At SpecialtyCare, we build and support the field of neurodiagnostics and know that our EEG technologists...Central Texas Perfusion Team Helps Save 19 Year Old
A Waxahachie teen survived a traumatic crash this year at the age of 19. His family...SpecialtyCare Highlight with Ovie Smith
This week, we’re highlighting one of our Intraoperative Neuromonitoring (IONM) clinical managers, Ovie Smith. She discusses...SpecialtyCare Joins NAW Week 2022!
National Apprenticeship Week (NAW) is a nationwide celebration to showcase the opportunities that Registered Apprenticeships offer...Robin Akins Attends Medical Mission to Trinidad
Recently, Robin Akins, from our Phoenix IONM Team, went on a medical mission to care for...CIM Week 2022 Highlight: Day in the Life, MIS Clinical Specialist Edition
We celebrate our first annual CIM Week this week, October 10-14, 2022. CIM stands for Comprehensive...Martin Glenn Receives CREF’s 2022 Swain Scholarship
SpecialtyCare's Martin Glenn Receives Cardiothoracic Surgery Symposium’s Top Award: The 2022 Swain Scholarship SpecialtyCare is thrilled...Now Hiring Perfusionists in Bristol, TN!
Is it time for you to get a change in scenery? If you’re reading this, you’re...Happy ECMO Week 2022 Highlights
ECMO Team Joins Team of Heroes in Saving a Life Florida resident, Don Brown, had a...Paris Parnell Attends Medical Mission to Dominican Republic
Recently, Paris Parnell, BS, CNIM, went on a medical mission to serve the Dominican Republic. We...Reasons to be a Surgical Neurophysiologist in Sacramento
Join Us in Sacramento! Can you see yourself working for SpecialtyCare? We can, too! Our IONM...The Importance of Patient Experience Through Proper Staffing
There's no easy way around it: staffing shortages are impacting patient safety and experience. A quality...Day in the Life: ATS & MIS Edition with Stephanie Nalley Levy
We’re highlighting some of our amazing SpecialtyCare staff. These individuals make a significant impact every day,...Sarah Lewis and Eduardo Bolorino Attend Medical Mission in the Dominican Republic
Sarah Lewis and Eduardo Bolorino Attend Medical Mission in the Dominican Republic The IONM Medical Mission...Vegas is Calling: Open Positions!
SpecialtyCare is currently hiring in Las Vegas, and we're throwing in a great benefits package, too....Studies Show Reduced Risks for Pediatric Scoliosis Patients
SpecialtyCare is the largest provider of intraoperative neuromonitoring (IONM) services in the nation with 130,000 cases...Patient, Procedural, and Practice Variables that Impact the Clinical Utility of IONM during Cervical Spine Surgery: A National Database Analysis
SpecialtyCare is an industry leader in data and research, teaming with surgeons in thousands of hospitals...2022 Winners of Brown-Brukardt Perfusion Scholarship
SPECIALTYCARE ANNOUNCES WINNERS OF THE 2022 BROWN-BRUKARDT PERFUSION SCHOLARSHIP Scholarship winners will receive a capped, one-time...SpecialtyCare Celebrates Women’s Health Week 2022
Women face unique health issues that present themselves differently than those of men. From May 8–May...Shannon Barletti, BSN, RN, CCP, Presents “Anticoagulant Use during Extracorporeal Membrane Oxygenation: A Comparison of COVID-19 and ARDS Patients” at AmSECT’s 60th International Conference
The 60th AmSect International Conference The 60th American Society of Extracorporeal Technology (AmSECT) International Conference was...SpecialtyCare’s Bryan Wilent, PhD, DABNM, FASNM, Announced as Incoming President for American Society of Neurophysiological Monitoring (ASNM)
We are thrilled to announce that beginning May 21, 2022 Bryan Wilent, Vice President of Quality...Patient Factors Impacting Baseline MEPs in Patients Undergoing Cervical Spine Surgery for Myelopathy or Radiculopathy
SpecialtyCare is an industry leader in data and research, teaming with surgeons in thousands of hospitals...The Impact of Inhalational Anesthetic Agents on the Baseline Monitorability of MEPs During Spine Surgery
SpecialtyCare is an industry leader in data and research, teaming with surgeons in thousands of hospitals...Sarah Witulski, Clinical Technician II, Saves the Day with Unrelenting Attention to Detail
Recently, Sarah Witulski, Clinical Technician II, made a wonderful impact on a spine ATS case. Energy...Linda B. Mongero, BS, CCP Emeritus, Publishes “A Survey of Women in the Perfusion Workforce: 2021”
The Research Abstract A 2011 survey was distributed to all female perfusionists in the United States,...Neurodiagnostic Week 2022: Celebrating SpecialtyCare’s EEG and TCD Technologists
Neurodiagnostic Week is an ASET event that honors neurodiagnostic professionals and the value they provide in...Day in the Life: Surgical Assist Edition with John Martinez
We greatly appreciate and value all of our SpecialtyCare Surgical Assist employees. In honor of Surgical...Research Shows Hospitals Who Publish Have Better Results
The primary function of a hospital is to provide direct patient care. They also educate future...Work for SpecialtyCare in Milwaukee, Wisconsin
For those of you out there who are already in the IONM field and looking for...Day in the Life: CVMT Edition
Our CVMT’s provide a wide range of services in multiple departments within hospitals. You’ll find CVMT’s...Day in the Life: ATS Edition with Kimberly Sharp
We greatly appreciate and value all of our SpecialtyCare ATS employees. We’re highlighting one of our...Day in the Life: ATS Edition with Stephen Watkins
We greatly appreciate and value all of our SpecialtyCare ATS employees. This week, we’re highlighting one...Fairfield Medical Center Continues to Thrive
Six months ago, we wrote about our team's success in the Central Sterile Department at Fairfield...SpecialtyCare Highlight with Toree Baldwin
This week, we’re highlighting one of our Intraoperative Neuromonitoring (IONM) clinicians, Toree Baldwin. She discusses what...Multi-Institutional Analysis of 505 COVID-19 Patients Supported with ECMO: Predictors of Survival
On February 18, 2022, The Annals of Thoracic Surgery published an important manuscript titled: “Multi-institutional Analysis...Day in the Life: HR Edition with Shandus Parish
We greatly appreciate and value all of our SpecialtyCare Human Resources employees. This week, we’re highlighting...IONM Use Reduces Opioid Rx, Readmissions
The opioid epidemic has become a national crisis, with over 300,000 deaths attributed to opioid overdose...Patient Safety Awareness Week 2022
Patient Safety Awareness Week is an annual recognition event intended to encourage everyone to learn more...Day in the Life: HR Edition with Julie Aebie
We greatly appreciate and value all of our SpecialtyCare Human Resources employees. This week, we’re highlighting...Day in the Life: ATS Edition with Tenesha Trammell
ATS plays a critical role in patient lives, and we’re incredibly fortunate to our SpecialtyCare team...Day in the Life: HR Edition with Sarah Dyczewski
We greatly appreciate and value all of our SpecialtyCare Human Resources employees. This week, we’re highlighting...SpecialtyCare: Your Leader for ECMO Services and Support
SpecialtyCare is the leader in perfusion, ECMO services, and patient blood management, performing over 130,000 procedures...The Truth About Autotransfusion
The truth is autotransfusion safely outperforms donor blood transfusions and significantly reduces costs for your hospital,...KPIs: What They Mean and Why They Matter
A key performance indicator (KPI) is a type of performance measurement, and KPIs evaluate the success...Jeffrey P. Jacobs, MD, FACS, FACC, FCCP, to Present Abstract at AATS 2022
Jeffrey P. Jacobs, MD, FACS, FACC, FCCP, will present an abstract on the Variation in Survival...Why Specialty Care Is the Top Choice for Your ECMO Needs
SpecialtyCare has increased its experience and national reach over the years, becoming a thought leader in...CIM: A Recurring Short-term Staffing Problem Equals a Long-Term Problem
The ongoing COVID-19 pandemic has caused overwhelming challenges in providing patient care and resulted in significant...Job Opening: Sterile Processing Technician in Richmond, VA
Are you looking for a new opportunity to advance your career with a great team? SpecialtyCare...Understanding Autotransfusion
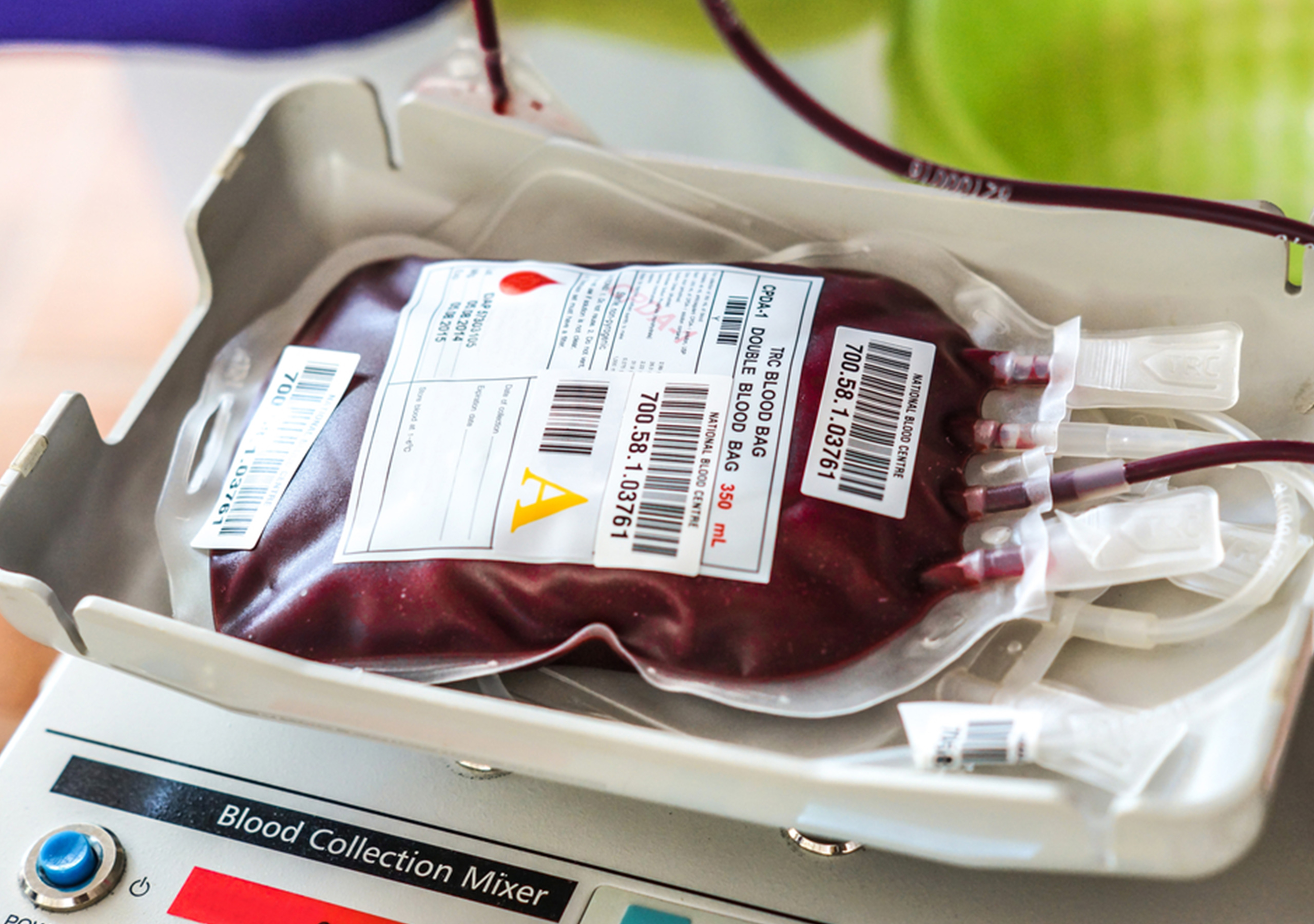
Every day, 250 highly skilled ATS clinical specialists work in operating rooms across the country to...Improve Your Patient Blood Management Program with Autotransfusion
There are twenty-one million blood components transfused every year in the United States. Autotransfusion is a...Blood Shortage Gets National Attention
COVID-19 caused overwhelming challenges to providing adequate medical care to patients, including a decline in donor...New Year, New Goals Pt. 3
SpecialtyCare has partnered with Harvard Business Publishing to launch the Harvard ManageMentor program, the most trusted...Dual MIS and ATS Role Needed in Santa Fe, NM
Are you looking for a new opportunity to work with a passionate, driven team in a...New Year, New Goals Pt. 2
SpecialtyCare has partnered with Harvard Business Publishing to launch the Harvard ManageMentor program, the most trusted...New Year, New Goals Pt. 1
SpecialtyCare has partnered with Harvard Business Publishing to launch the Harvard ManageMentor program, the most trusted...SpecialtyCare Honors Martin Luther King Jr. Day
Every January, we celebrate the lasting legacy of Dr. Martin Luther King Jr. We know him...SpecialtyCare Highlight with Ed DeLaney and Dr. Derek Brinster
Todd Schlosser sat down with Ed DeLaney, the Director of Perfusion at Northwell Health, and Dr....SpecialtyCare Receives Cigna Well-Being Award
Every year, Cigna selects a group of organizations for the Cigna Well-Being Award to honor the...SpecialtyCare Highlight with Ruggero Bruzzone
This week, we’re highlighting one of our ECMO Coordinators, Ruggero Bruzzone. He details his journey to...SpecialtyCare’s Shannon Clark on Medical Mission to Jamaica
SpecialtyCare’s Shannon Clark recently participated in a medical mission trip to Jamaica. She details how she...Valuing Others with Our Actions, Vol. 1
SpecialtyCare is honored to share that one of our patients at Swedish Medical Center, Nate McWilliams,...SpecialtyCare Highlight with Stephanie Adamski, EEG Clinical Manager
Stephanie Adamski, our EEG Clinical Manager, is the lead singer for the band Midheaven, and they...Day in the Life: MIS Edition with Suni Sullivan
Throughout Minimally Invasive Surgery (MIS) Week, we’re highlighting some of our amazing SpecialtyCare staff. These individuals...Day in the Life: MIS Edition with Brittany Barbee
Throughout Minimally Invasive Surgery (MIS) Week, we’re highlighting some of our amazing SpecialtyCare staff. These individuals...Day in the Life: MIS Edition with LaKesha King
Throughout Minimally Invasive Surgery (MIS) Week, we’re highlighting some of our amazing SpecialtyCare staff. These individuals...Day in the Life: MIS Edition with Shauntra Dickerson
Throughout Minimally Invasive Surgery (MIS) Week, we’re highlighting some of our amazing SpecialtyCare staff. These individuals...SpecialtyCare Celebrates MIS Week
SpecialtyCare is proud to celebrate its second Minimally Invasive Surgery (MIS) Week. We have more than...Harvard ManageMentor
SpecialtyCare has partnered with Harvard Business School to launch the ManageMentor program, the most trusted on-demand...Gregory Agoston Featured in November HPN Edition
Recently, many sterile processing departments (SPDs) have implemented disposable/single-use-only endoscopic devices. There has been media buzz...Managing Stress Reactions with Self-Care Strategies
Experiencing a traumatic event can lead to various stressors. Each individual processes trauma differently, resulting in...How Fairfield Medical Center Tackles Sterile Processing
Fairfield Medical Center's Sterile Processing Department recently discussed the realm of sterile processing, everyday responsibilities, the...SpecialtyCare Celebrates Medical Staff Services Awareness Week
In 1992, George W. Bush signed a Congressional House Joint Resolution declaring a week of November...SpecialtyCare Celebrates Allied Health Professionals Week
The week of November 7-13 celebrates Allied Health Professionals Week. The U.S. employs over 8 million...SpecialtyCare Highlight with Artem Zhosan
Artem Zhosan is an ECMO specialist at SpecialtyCare, currently working in the Los Angeles area. Here,...AmSECT Announces Winners of the SpecialtyCare Medical Mission Fund
AMSECT ANNOUNCES RECIPIENTS OF THE 2021 SPECIALTYCARE MEDICAL MISSION FUND Three students will receive the $25,000...How to Handle the Post-Pandemic Challenges of the Sterile Processing Department
How to Handle the Post-Pandemic Challenges of the Sterile Processing Department Like all hospital departments, the...SpecialtyCare Highlight with Dr. Stephen Griffith
Seeking a Career in Healthcare Dr. Stephen Griffith is a board-certified neurosurgeon whose interest in becoming...SpecialtyCare Celebrates Medical Assistant Recognition Day
Medical assistants are one of the fastest-growing professions in the nation. These individuals play a valuable...Sterile Processing Week Feature with Randalyn Walters, SpecialtyCare’s Clinical SPD Educator
Sterile Processing is a distinct health profession that focuses on the direct support of patients who...SpecialtyCare Celebrates SPD Appreciation Week
Sterile processing is the cleaning, inspecting, disinfecting, and sterilization of surgical medical instruments and equipment. It’s...Top 5 Reasons to be a Surgical Neurophysiologist in Philadelphia
Great news for surgical neurophysiologists reading this right now. SpecialtyCare is currently hiring in Philly. If...SpecialtyCare Leads ECMO Training at Swedish Hospital
To continue highlighting ECMO Appreciation Week, we want to raise awareness for the importance of this...SpecialtyCare Highlight: Jonathan Rasouli, MD
During an episode of Checking the Vitals this year, SpecialtyCare's Todd Schlosser sat down with Jonathan...The Effect of COVID-19 on Adult Cardiac Surgery
The Effect of COVID-19 Adult Cardiac Surgery in the United States in 717,103 Patients Abstract: The...SpecialtyCare Celebrates Health Unit Coordinator Day
SpecialtyCare is proud to celebrate Health Unit Coordinator Day on August 23, 2021. This day is...Perfusion Leaders Now Available!
SpecialtyCare is thrilled to announce the launch of the Perfusion Leaders website this week! Perfusion Leaders...Surgical Neurophysiologist Needed in Mobile, Alabama
Are you looking for a unique opportunity to work with one of the most experienced IONM...SpecialtyCare Celebrates National Health Center Week
This year, SpecialtyCare is proud to celebrate National Health Center Week from August 8-14! National Health...SpecialtyCare’s Own Bart Hensler in Tanzania
Recently, one of SpecialtyCare’s pediatric perfusionists participated in a medical mission trip to Tanzania. Bart Hensler,...Life in the OR: William Edwards, Sr. Anesthesia Tech
Anesthesia technology is a distinct health profession that focuses on the necessary clinical procedures that assist...Life in the OR: Stephen Edgett, Anesthesia Tech
Anesthesia technology is a distinct health profession that focuses on the necessary clinical procedures that assist...Day in the Life: Perfusion Assistant Edition
In honor of Anesthesia Tech and CVMT Appreciation Week 2021, we wanted to showcase another inside...Day in the Life: Cardiovascular Monitoring Technician Edition
Our CVMT’s provide a wide range of services in multiple departments within hospitals. You’ll find CVMT's...SpecialtyCare Celebrates Anesthesia Technology and CVMT Appreciation Week
SpecialtyCare is proud to celebrate Anesthesia Technology and CVMT Appreciation Week. These individuals are on the...Multi-institutional Analysis of 200 COVID-19 Patients treated with ECMO: Outcomes and Trends
An abstract has been written for submission to the Eastern Cardiothoracic Surgical Society 2021 Meeting, to...An Effective IONM Program is Critical for Your OR
At SpecialtyCare, we value the health and safety of our patients. As a partner in intraoperative...World Brain Day 2021
July 22 marks World Brain Day. This year’s theme is Multiple Sclerosis, which invites those living...SpecialtyCare Resources
We continue to be proud of the work our team completes every year. SpecialtyCare is dedicated...Shannon Barletti Receives The 2021 Swain Scholarship
SpecialtyCare Perfusionist Shannon Barletti Receives Cardiothoracic Surgery Symposium’s Top Award: The 2021 Swain Scholarship SpecialtyCare is...Surgical Neurophysiologist Needed in Boston, Massachusetts
Are you looking for a new opportunity to provide patient care with one of the most...The Effects of a National Blood Shortage
COVID-19 caused overwhelming challenges when it came to providing medical care to patients. As the pandemic...SpecialtyCare Covers AmSECT Membership for Perfusion Service Line
SpecialtyCare is excited to announce a new partnership with the American Society of Extracorporeal Technology (AmSECT)...Surgical Neurophysiologist Needed in Medford, Oregon
Are you looking for a unique opportunity in southern Oregon to provide patient care in a...The Top 4 Capabilities of Effective Leaders
Transitioning into a leadership role poses unique challenges. Across all industries, these four competencies are what...Which Competencies Should Your SPD Have?
It’s a primary goal for sterile processing departments to operate at peak efficiency while maintaining the...Surgical Procedures Supported by SpecialtyCare
As a partner in IONM, we are your insurance policy against risk and the high cost...SpecialtyCare Honors Men’s Health Week
This June, we’re proud to celebrate Men’s Health Week, which draws awareness to male health issues...SpecialtyCare Celebrates National Nursing Assistants Week
This year, we celebrate the 44th annual National Nursing Assistants Week from June 17-24, which spotlights...Life in the OR: Surgical Neurophysiologist Edition, Vol.3
Our IONM training program welcomes up to 25 new students across four training cohorts each year....The Mental Health Benefits of Going Outdoors This Summer
Everyone has struggled with their mental health in some capacity during COVID-19, acclimating to a new...When Surgical Demand Returns, How Will Hospitals Manage Their Growing Backlog?
Nearly a year into the COVID crisis, hospitals are continuing to have to postpone elective surgeries....Perfusionists Needed in Detroit, MI
Are you looking for an excellent opportunity to join a supportive team of talented professionals? We’re...SpecialtyCare Announces Christy Kisner as President of Intraoperative Neuromonitoring and Neurodiagnostic Services
June 10, 2021, (Brentwood, TN)-SpecialtyCare, the nation’s leading provider of Intraoperative Neuromonitoring (IONM), Perfusion, and Surgical...How to Be an Effective SPD Manager
The Sterile Processing Department’s primary goal is to streamline management processes, so your operating room can...Life in the OR: Surgical Neurophysiologist Edition, Vol.2
Our IONM training program welcomes up to 25 new students across four training cohorts each year....A Comprehensive Guide to Perfusion
Perfusionists genuinely are the heart of the operation. Hospitals must meet the needs of 340,000 patients...The Top 5 Ways to Eliminate Surgical Delays
Sterile processing is one of the most critical departments within any healthcare facility. However, it often...In Loving Memory of Jonathan Walters
Dear SpecialtyCare Friends, It is with a heavy heart and tremendous sense of loss that I...Life in the OR: Surgical Neurophysiologist Edition, Vol.1
Our IONM training program welcomes up to 25 new students across four training cohorts each year....How Sterile Is Your Processing?
Sterile processing is a critical component in ensuring the safest patient care before, during, and after...The Mental Health Benefits to Making a Career Change
People sometimes experience aspects of their job that can lead to a negative impact on their...Job Opening: Surgical Neurophysiologist in Pensacola, Florida
Are you looking for a new opportunity to work with a passionate and driven team in...Celebrating EMSC Day 2021
Children respond differently than adults do to injury and illness, and those differences can be seen...SpecialtyCare Honors Mental Health Awareness Month
5 Ways to Maintain Your Mental Health in the Medical Field A negative stigma often surrounds...SpecialtyCare Celebrates National Nursing Month
The History of Nursing: An Overview Today’s healthcare system houses 3.1 million nurses who provide valuable...Job Opening: Surgical Neurophysiologist in Seattle, Washington
Are you looking for a new opportunity to join an experienced team with the potential to...SpecialtyCare Celebrates Women’s Health Week
Women face unique health issues that present themselves differently than those of men. From May 9–May...2021 Winners of Brown-Brukardt Perfusion Scholarship
SPECIALTYCARE ANNOUNCES WINNERS OF THE 2021 BROWN-BRUKARDT PERFUSION SCHOLARSHIP Three perfusion school students and two clinical...Honoring the History of Open-Heart Surgery with a Heart-Lung Machine
Perfusionists are at the heart of the operation and provide much needed assistance during cardiac surgery,...SpecialtyCare Team Dedicates Work to Published Research for COVID-19 Patients
Multi-institutional Analysis of 100 Consecutive Patients with COVID-19 and Severe Pulmonary Compromise Treated with Extracorporeal Membrane...Celebrating Perfusion Week
What is Perfusion Week? Perfusion Week 2021 takes place from May 2-8 and commemorates the work...How Intraoperative Neuromonitoring Makes Surgery Safer
What is Intraoperative Neuromonitoring? Intraoperative neuromonitoring protects a patient during spinal surgery by monitoring and evaluating...Al Stammers to Receive The John H. Gibbon Jr. Award
SpecialtyCare is thrilled to celebrate Al Stammers, MSA, PBMS, CCP Emeritus, as the 2021 recipient of...Perfusion Equipment Purchase and Lease
The primary objective for hospitals is to provide high-quality patient care, increase efficiency, and reduce costs....The History of Neurodiagnostics
What is Neurodiagnostics? Neurodiagnostics is recording electrical activity in the brain, central nervous system, and peripheral...Neurodiagnostic Week 2021: Celebrating SpecialtyCare’s Deep Brain Stimulation Team
SpecialtyCare’s Nicole Young, PhD & Dr. Rezai fine-tuning an implant (Greg Ellis/WVU Photo) Today we recognize...Neurodiagnostic Week 2021: Celebrating SpecialtyCare’s EEG and TCD Technologists
By bringing to light what’s hidden from sight, SpecialtyCare’s EEG & TCD Technologists are the vital...Managing Disposable Consignment Inventory
A common theme across many hospitals is unused inventory. Hospitals heavily stock their shelves with perfusion...Job Opening: Perfusionist in Richmond, Virginia
Are you looking for a new opportunity to advance your career with a great team? SpecialtyCare...Job Opening: Perfusionist in Bristol, Tennessee
Are you looking for a new opportunity to join an experienced team with a generous sign-on...Job Opening: Perfusionist in Houston, Texas
Are you looking for a new opportunity to join an experienced team with a generous sign-on...Job Opening: Perfusionist in Reading, Pennsylvania
Are you looking for a new opportunity to advance your career with a 20k sign-on bonus?...Celebrating World Health Day
April 7th marks the celebration of World Health Day. Every year, the World Health Organization (WHO)...Job Opening: Perfusionist in Harrisburg, Pennsylvania
Are you looking to join an experienced team and earn a 25k sign-on bonus? SpecialtyCare is...Celebrating National Doctor’s Day
The healthcare industry has evolved significantly over the last couple of decades. With advancements in research...Women’s History Month: Celebrating Dr. Antonia Novello
Dr. Antonia Novello is a physician and public health administrator. She was appointed the 14th Surgeon...Job Opening: Perfusionist in Ocala, Florida
Are you looking for a new opportunity to join an experienced team and advance your career?...Women’s History Month: Celebrating Mary Edwards Walker
Mary Edwards Walker was the first woman in the United States to earn a medical degree....Job Opening: Perfusionist in Lewes, Delaware
Are you looking for a new opportunity to join an experienced team with a 20k sign-on...Job Opening: Perfusionist in Morristown, New Jersey
Are you looking for a new opportunity to join an experienced team and advance your career?...Celebrating Healthcare HR Week Part 2: HR Business Partner, Credentialing, Compensation Business Partner
Healthcare Human Resources Week – the third week of March – is designated to recognize human...The Importance of Active Listening Skills in Business Communication
A common misconception is that communication is only talking but the second part of that equation...An Inside Look at Life in the Operating Room
Are you passionate about helping people? If so, a career in the medical field might be...The Importance of Business Communication in Leadership
Business communication is the process of sharing information between employees within and outside of the company...Celebrating Healthcare HR Week Part I: Recruiting and SpecialtyCare University
Healthcare Human Resources Week – the third week of March – is designated to recognize human...Job Opening: Perfusionist in Marshfield, Wisconsin
Are you looking for the opportunity to advance your career with a great team? SpecialtyCare is...Job Opening: Perfusionist in Terre Haute, Indiana
Are you looking for the opportunity to advance your career with a great team? SpecialtyCare is...Job Opening: Surgical Neurophysiologist in Rancho Cucamonga, California
Are you looking for a new opportunity to join an experienced team with the potential to...Women’s History Month: Celebrating Elizabeth Blackwell
Elizabeth Blackwell was the first woman to earn a medical degree in America. She was a...Job Opening: Perfusionist in Albuquerque, New Mexico
Are you looking for the opportunity to advance your career with a great team? SpecialtyCare is...Job Opening: Perfusionist in Loma Linda, California
Are you looking for the opportunity to advance your career with a great team? SpecialtyCare is...Job Opening: Perfusionist in Detroit, Michigan
Are you looking for the opportunity to advance your career with a great team? SpecialtyCare is...Honoring Women’s History Month Through the Lens of Allied Health Professions
For decades, men have represented a majority of the healthcare industry. However, there are many women...Q&A with Julie Trott and Kristina Young, Directors of our IONM SNI Training Program
We sat down with Kristina Young and Julie Trott to share answers to some of the...SpecialtyCare’s Presentation at the 2021 Society of Thoracic Surgeons Meeting on COVID-19 and ECMO Featured in MedPage Today. Results From Our National Experience Reaffirms ECMO as a Strategy for COVID-19 Patients with Severe and Medically Refractory Respiratory Problems
SpecialtyCare is honored to share that our research and presentation titled: “Analysis of 189 Consecutive Patients...Announcing the 2021 Brown-Brukardt Perfusion Scholarship Program! SpecialtyCare is Pleased to Award an Additional Scholarship This Year, Bringing the Total to Five
As the largest provider of perfusion services in the country, SpecialtyCare values the critical team- role...Job Opening Alert: Surgical Neurophysiologist in Bakersfield, California
Looking for new places to explore, a team you can count on, and the opportunity to...Job Opening Alert: Surgical Neurophysiologist in Los Angeles, California
Looking for a change of scenery, a trustworthy team, and greater earning potential? SpecialtyCare is seeking...SpecialtyCare’s COVID-19 and ECMO Research Selected for Presentation During the Southern Thoracic Association’s (STSA) Special Edition Webinar on November 5, 2020; Open to All Healthcare Professionals
SpecialtyCare is honored to share that our abstract entitled: “Experience with 46 patients with COVID-19 and…
How to Assess IONM Providers for Your OR
Like many surgeons and hospitals, you know the efficacy of intraoperative neuromonitoring (IONM). Your pre-work has…
Turn Your “Cost Center” SPD into a Revenue Generator
An underperforming sterile processing department (SPD) can be the source of dramatic hidden costs, both financially…
How to Assess Perfusionists for Your OR
Heart surgeries are more complex than ever. To ensure the best patient outcomes, perfusionists should meet…
Don’t stress out your perfusionists, consider starting an ECMO program!
Data suggests that there will continue to be a perfusion shortage across the entire United States….
Advocating for Safer Surgery- Principle #4: Sterilization
Every day, healthcare facilities’ sterile processing departments handle thousands of reusable surgical instruments and devices. The…
“Inside the Fight to Save Houston’s Most Vulnerable” Q&A with Kirti Patel, SpecialtyCare’s National Clinical Specialist/Perfusion Clinical Manager at Houston Methodist Hospital
SpecialtyCare is honored to be a partner of Houston Methodist Hospital, working alongside their medical teams…
Advocating for Safer Surgery-Principle #3: Blood Transfusion Reduction
Some providers have learned that balancing both clinical and economic concerns must begin on the most…
SPD Specialization is Becoming a Necessity
Innovations in healthcare have outpaced the generalized sterile processing department capabilities. Rapid advancement in surgical procedures…
An OR Leader’s Introduction to Making Surgery Safer with IONM.
What is Intraoperative Neuromonitoring or IONM? Intraoperative neuromonitoring (IONM) is the continuous surveillance of a patient’s…
Advocating for Safer Surgery- Principle #2: Staff Retention
Healthcare is a labor-driven service that depends on the talent and competencies of each member of…
Advocating for Safer Surgery- Principle #1: Communication
In surgical teams, health professionals are highly interdependent and must work under time pressure. It is…
Advocating for Safer Surgery: Four Principles
With over 300 million people worldwide going under the knife every year, safer surgery is a…
World Brain Day 2020 | Raising Awareness for Parkinson’s Disease
SpecialtyCare is honored to be joining the World Federation of Neurology and the International Parkinson and…
Action Speaks Louder Than Words: Our Values Blog Series | Integrity
We know that it’s not enough for an organization to simply state its values. We are…
Partnering with Highly-Trained Clinicians Starts with the Provider’s Commitment to Resources and Education
Offering excellent IONM services starts with the hiring and training process. There are only a very…
Action Speaks Louder Than Words: Our Values Blog Series | Sense of Urgency
We know that it’s not enough for an organization to simply state its values. We are…
SpecialtyCare’s COVID-19 and ECMO Research Selected for the Opening Presentation of the First Scientific Session at The Southern Thoracic Association’s (STSA) 67th Annual Meeting in November
SpecialtyCare is honored to share that our abstract entitled: “Experience with 46 patients with COVID-19 and…
ECMO and COVID-19 Webinar Draws Large Attendance as Healthcare Providers Continue to Seek Information on ECMO for Patients with COVID-19
SpecialtyCare recently hosted two educational webinar opportunities for perfusionists and critical care physicians. Both sessions were…
Credentialing for Life-Saving Care: Q&A with Jessica Campbell
We sat down with Jessica Campbell, SpecialtyCare’s Manager of the Credentialing Department to learn about the…
How to Increase Satisfaction and Become the Provider of Choice
How can we as surgical neurophysiologists improve a patient’s experience and surgeon satisfaction? At SpecialtyCare, it…
Starting an In-House ECMO Program Makes Sense, but Support is Critical
The research is there — ECMO programs are saving lives on a more frequent basis. But…
SpecialtyCare to Host Webinar for Perfusionists Regarding ECMO and Treatment of COVID-19 on June 4th, Including Opportunity for Continuing Education Credit
SpecialtyCare continues to place an important focus on sharing our published research on the role of…
Q&A with Awilda Rivera, Manager of the Scheduling Department at SpecialtyCare
We sat down with Awilda Rivera, SpecialtyCare’s Manager of the Scheduling Department to learn about the…
How Do You Ensure You Always Have Perfusion Support at Your Hospital, Without Over or Understaffing?
The need for perfusion services is rising due to the decrease of available perfusionists and the…
Q&A with Andrew Goldstein, Manager of Biomedical Engineering at SpecialtyCare
The biomed technicians of SpecialtyCare are maintaining their usual high standards, despite the challenges involved in…
SpecialtyCare Medical Department Collaborates with The American Society for Artificial Organs (ASAIO) on Research to Understand the Role of ECMO in the Management of COVID-19
SpecialtyCare’s real-time cohort of 32 patients across 9 states over 24 days is the largest published…
How COVID-19 Has Impacted Sterile Processing Departments: Input from the Experts
Sterile processing has always had a uniquely important role in the hospital, all the more so…
Join Our Augusta Perfusion Team!
The need for healthcare professionals has never been greater. We are proud to be working with...COVID-19 and Healthcare Workers: Future ACNP Talks Graduation Prospects, Work in the COVID Unit
Lauren Bosch, a 30-year old nurse in Fayetteville, Arkansas, is an RN studying to become an…
Special COVID-19 Episode with Kirti Patel
Today, our guest is Kirti Patel, the National Clinical Specialist for Perfusion at SpecialtyCare. In this…
Special COVID-19 Episode with Courtney Petersen
In this special episode, we focus on the COVID-19 outbreak that is currently happening in the…
Life in the OR During COVID-19 Pandemic: A Clinician’s Perspective
This pandemic has us living in a dynamic and intense time, globally and in healthcare specifically….
Training in the Midst of COVID-19
It is certainly an uncertain time in our nation, and we are relying on healthcare workers…
5 Ways to Deal with Stress, Anxiety, & Fear During the COVID-19 Crisis (or Other Adverse Circumstances)
As the world deals with the fallout from the COVID-19 pandemic, many of us are wrestling…
SpecialtyCare Extends Perfusion Scholarship Deadline
New Application Deadline, April 22, 2020 This has been a challenging time for everyone and our…
A Message from SpecialtyCare
As healthcare providers, we understand that this is a challenging and uncertain time for everyone. We…
We Need More Healthcare Heroes: Join Our Denver Perfusion Team
Our country is facing unprecedented times, and need healthcare professionals – the heroes on the front…
SpecialtyCare IONM Teams Up with PENCIL
PENCIL Foundation is a premier organization in Nashville that provides a unique opportunity for Metro Nashville…
Can Our Perfusion Services Enhance Your OR?
When it comes to innovation in the OR, SpecialtyCare works to stay on the leading edge…
SPECIALTYCARE’S BIOMED TECHS COME TOGETHER AT AIRPARK TECHNICAL CENTER
In early February, members of the two teams that make up SpecialtyCare’s biomedical department convened at…
How We Train & Support Perfusionists to Provide High-Quality Services to the OR
Perfusion services are in high demand as the number of cardiac surgeries increases and the uses…
Join our Orlando IONM Team
Good news for all you IONM specialists out there. SpecialtyCare has an open neurophysiologist position in...IONM Jobs in Albuquerque, New Mexico
SpecialtyCare continues to grow and expand into new markets and with this expansion, comes the need...How a Neurophysiologist Impacts Patient Care
The surgical neurophysiologist functions as the patient’s advocate at every level. This role requires a high…
Perfusion: The Heart of the Operation
Perfusion is a vital part of cardiac surgeries, but many people are still unaware of what…
From Lifeguard to Neurophysiologist: Megan Neckelmann Enjoying Life in the OR
Like many of our IONM clinicians, the field of intraoperative neuromonitoring wasn’t Megan Neckelmann’s radar originally….
IONM Data and Innovation
SpecialtyCare stands out from the competition in the intraoperative neuromonitoring (IONM) space in a number of…
IONM: Making Surgery Safer
SpecialtyCare is proud to offer intraoperative neuromonitoring (or IONM) services for hospitals and clinics nationwide. In…
Perfusion Data and OR Innovation: How Our Research Database Is Facilitating Safer Surgery
Perfusion is a vital and continually developing field, one that is instrumental to the overall efficacy…
A Day in the Life of a Neurophysiologist
“Medicine is a science of uncertainty and an art of probability.”—William Osler. This statement sums up…
SpecialtyCare Acquires Phoenix Perfusion Services and Arizona Perfusion Supply Company
This merger increases SpecialtyCare’s market leadership as the nation’s largest, most comprehensive provider of perfusion services,…
Past Perfusion Scholarship Winner Grateful for Life in the OR
Like many Biomedical Chemistry majors, Cassie Lopez had intentions of going to medical school after graduation….
DENVER PERFUSION CAREERS
Let’s be honest, everyone and their mother has thought about moving to Denver, Colorado at some...Kim Hall Finds More Than a Career in IONM
When I joined SpecialtyCare and graduated from the SNI training program, I was excited to enter…
Announcing 2020 Brown-Brukardt Perfusion Scholarship
UPDATE: Due to the circumstances surrounding the COVID-19 Pandemic, we have extended our Application Deadline to…
Benefits of Joining the SpecialtyCare Team
Becoming a medical professional is an expensive endeavor. You’ve worked hard to get where you are...Happy 30th to the Salem Health Cardiac Program
SpecialtyCare would like to congratulate Salem Health for 30 years of cardiac surgery excellence. The cardiac…
What Is Bloodless Perfusion, and Why Is It Important?
Perfusion is the circulation of blood to organs and tissues in the body, which provides them…
SPECIALTYCARE ACQUIRES INTRAOPERATIVE NEUROMONITORING PROVIDER SYNAPSE
Deal increases market leadership as the nation’s largest, most comprehensive provider of intraoperative neuromonitoring November 19,…
Neurosurgeon Shares Wisdom with New Neurophysiologists
“Speak loudly, clearly and confidently. Your delivery is a big part of the message.” Neurosurgeon Dr….
Tony Brown’s “Good Catch” Saves the Day
For this edition of Life in the OR, we are thrilled to highlight Anthony (Tony) Brown,…
IONM Training Program Wins Malcolm Knowles Award
The SpecialtyCare is proud to announce that our IONM training program has been selected as the…
SpecialtyCare Perfusionist Wins Utley Award at CREF 2019
Congratulations to Yajun Ren, PhD, CCP, LP, perfusionist for SpecialtyCare, for receiving the Utley Award at…
Chiropractors Find New Career in the OR
In healthcare, sometimes a career change can provide the mental boost someone needs to avoid burnout,…
Career Change Restores Work-Life Balance for SpecialtyCare Associate
Jodi Parsons, DC, CNIM Jodi Parsons was in private chiropractic practice with her husband for just…
Sterile Processing Problems: High Turnover in Hospital SPD Staff
In a comparison with other high-income countries, the United States spends the most on healthcare —…
Sterile Processing Problems: How the Increase in Complex Instruments Affects Cleaning Efficacy
In a comparison with other high-income countries, the United States spends the most on healthcare —…
Perfusion Certification Exam Breakdown
If you’re already in perfusion school or considering a career in perfusion, you might already be…
From Chiropractor to Surgical Neurophysiologist – A Great Move
Dan Filipkowski, DC, CNIM, D.ABNM “You just made that up, didn’t you?” That’s what Dan Filipkowski…
Sterile Processing Problems: HAI & SSI Rates Caused by Dirty Instruments
We all know that disease can be transmitted in many ways in a hospital, but some…
Dr. Suken Shah on How IONM Makes Surgery Safer
Intraoperative neuromonitoring (IONM) is a surgical innovation that monitors the electrical potential of nerves, allowing surgeons…
SpecialtyCare Marketing to Host Healthy Brand Webinar Series
Perception is reality. As a healthcare professional, developing a strong online presence backed with client referrals…
Cardiopulmonary Bypass, Perfusion and ECMO…What’s the Difference?
For people who aren’t already in the healthcare field, it can be mighty confusing to decipher…
What It Means To Be Patient-Centered
If you visited the main services pages on our website already (and you probably have if…
Saving Spines One Child at a Time
Sometimes you just need to make a bold move to get your life moving in the…
Maximizing OR Efficiency: What’s the Best Solution for Hospitals?
Time in the operating room has a significant effect on revenue and costs for hospitals. In…
Med School or Perfusion? Weighing Your Options
Every year in the United States, around 50,000 college students apply to medical school. In the…
Beating Night Shift: Tips for New OR Staff
As newcomers on the surgical team, there’s no doubt that many of you will be scheduled…
Top 3 Reasons to Work in Allied Health
When talking about jobs in the healthcare profession, seemingly vague-sounding terms like “allied health” can be…
From Soldier to Perfusionist – Erin Friesenborg’s Life in the OR
If at first you don’t succeed…. This proverb is one Erin Friesenborg knows all too…
IONM Openings in Raleigh, NC. Why You Should Consider a Move
If you’re a certified surgical neurophysiologist reading this right now (and there’s a decent chance you...The Importance of Sterile Processing
The U.S. healthcare system spends almost $10 billion dollars every year treating the top Hospital Associated…
Why You Should be a Neurophysiologist in Portland
Portland, Oregon. The western land of the hip and friendly. It’s currently ranked in the “Top...IONM Careers in Ocala, Florida
You may have never heard of Ocala before, but if you’re a neurophysiologist- and chances are...An Important Message from our CEO, Sam Weinstein
As the CEO of SpecialtyCare (and as a surgeon), I feel it is imperative that I…
Life in the OR – Kerry Cultice Dodds, CNIM, R. EEG T.
To say that Kerry Cultice Dodds is busy would be quite an understatement. She’s a mom,…
Top Reasons to be a Neurophysiologist in Northern Virginia
SpecialtyCare is currently hiring for IONM positions in the northern Virginia region. If you’re already a…
Reasons to be a Perfusionist in Albuquerque, New Mexico
So, there’s a very decent chance you’ve seen parts of Albuquerque, New Mexico already in the...Why Autotransfusion Is Safer and More Cost-Efficient than Donated Blood Transfusions
Blood transfusion is widely considered to be a beneficial treatment, but the American Medical Association and…
Reasons to be a Perfusionist in Shreveport
Shreveport, Louisiana. With gorgeous southern weather, charming locals and out-of-this-world food, it’s easy to see why...Four Reasons to be a Perfusionist in Washington D.C.
SpecialtyCare is currently hiring for a perfusionist in our nation’s capital. Chances are you’ve probably visited...Reasons to be a Neurophysiologist in Falls Church, Virginia
SpecialtyCare is currently looking for IONM specialists for a surgical neurophysiologist position in Falls Church, Virginia....Four Reasons to be a Neurophysiologist in New Orleans
New Orleans, Louisiana. Everyone’s familiar with The Big Easy in some way or another, whether it...Top Reasons to be a Perfusionist in Cape Girardeau
Cape Girardeau, Missouri. Chances are you never heard of this charming city before, but that’s all...Top Reasons to be a Perfusionist in Rehoboth Beach
SpecialtyCare is currently hiring for a perfusionist in Rehoboth Beach, Delaware. Chances are you’ve never heard...Reasons to be a Perfusionist in San Bernardino
SpecialtyCare is currently hiring for a perfusionist in San Bernardino, California. We’re even throwing in a...SpecialtyCare University Hits Milestone: 100 IONM Grads
We are thrilled to announce the SpecialtyCare IONM training program has graduated its 100th associate. This…
SPECIALTYCARE NEUROPHYSIOLOGISTS PLAY INTEGRAL ROLE IN FIRST AWAKE BRAIN SURGERY IN DELAWARE
June 7, 2019 (Brentwood,TN)—SpecialtyCare—the nation’s leading provider of outsourced intraoperative neuromonitoring (IONM) services—is pleased to announce…
Four Reasons to be a Neurophysiologist in West Palm Beach
It doesn’t get much better than West Palm Beach, Florida. Luckily for all you IONM specialists…
Top 4 Reasons to be a Neurophysiologist in Miami
SpecialtyCare is currently hiring for surgical neurophysiologists in Miami, Florida. You read that right. If you’re...Top 4 Reasons to be a Neurophysiologist in Baltimore
If you’re a neurophysiologist reading this and you’re thinking about switching things up in your life,...Four Reasons to be a Neurophysiologist in Lexington
For you neurophysiologists reading this who are thinking about a locale change and favor a medium-sized...Reasons to be a Perfusionist in Terre Haute
Terre Haute, Indiana. When you take a look at downtown Terre Haute, you can’t help but...Join our Team in Tallahassee
SpecialtyCare is currently looking for IONM specialists who are interested in moving to Florida. We have...Why You Should be a Perfusionist in Mishawaka, Indiana
Reasons to be a Perfusionist in Mishawaka Yep, that's right. You may have never heard of...Top 5 Reasons to Become a Surgical Neurophysiologist
If you’re looking at your medical career options, you have a number of good reasons to…
Salvaging Patients’ Blood During Cardiac Surgery Can Be Good for Their Recovery
The study, “The Influence of Intraoperative Autotransfusion on Postoperative Hematocrit after Cardiac Surgery: A Cross-Sectional Study,”…
Performance-Based Assessment of Oxygenators Used During Cardiac Surgery
Findings of the study, “Goal-Directed Perfusion Methodology for Determining Oxygenator Performance during Clinical Cardiopulmonary Bypass,” were…
Top 5 Reasons to be a Neurophysiologist in Boston
SpecialtyCare is currently hiring for a neurophysiologist position in Boston. If you’re reading this and are...Four Reasons to be a Neurophysiologist in Seattle
For you IONM specialists reading this, we have great news. SpecialtyCare is hiring for a surgical...Top 5 Reasons to be a Surgical Neurophysiologist in Jacksonville
Jacksonville, Florida. You’ve seen and heard about it in countless movies and TV shows as a...ECMO Frequently Asked Questions
We’ve talked a lot about what ECMO does on our website and in our blog section,…
Important Perfusion Organizations to Know
If you’re thinking about a career as a perfusionist, there is a tremendous abundance of resources…
Top 5 Reasons to be a Neurophysiologist in Daytona
If you’re a trained and certified neurophysiologist with experience under your belt in the IONM field,...Top 5 Reasons to be a Neurophysiologist in Atlanta
Atlanta, Georgia. Everybody knows of it, and chances are you may have even visited once or...Real-Time Monitoring Improves Safety for Patients on Heart-Lung Machine
Study findings were detailed in the article “Will Real-Time Monitoring Technology be a Game Changer for…
Cardiac Surgery Patients Benefit From Pairing of Two Blood Conservation Methods
The study, “The effectiveness of acute normolvolemic hemodilution and autologous prime on intraoperative blood management during…
The History of Perfusion
The history of perfusion dates back nearly 200 years. Perfusion can’t be credited to a single…
Top 5 Reasons to be a Neurophysiologist in Philadelphia
Great news for neurophysiologists reading this right now. SpecialtyCare is currently hiring in Philly. If you’re...ECMO Saves Lives of All Ages
For those of you that aren’t yet familiar with ECMO, you’re in the right place. While…
SPECIALTYCARE ANNOUNCES WINNERS OF BROWN-BRUKARDT PERFUSION SCHOLARSHIP
Three perfusion school students and one clinical technician will receive a one-time, $20,000 award April 29,…
Some Careers Aren’t Planned: Sylvana McIntyre’s Path to Perfusion
Happy Perfusion Week! I am Sylvana McIntyre, one of five perfusionists that have recently joined a…
What’s It Like to Be a Surgical Neurophysiologist in Denver?
As a surgical neurophysiologist seeking great job opportunities, you would do well to consider moving to...SPECIALTYCARE ACQUIRES INTRAOPERATIVE NEUROMONITORING PROVIDER NEUROPATH
Deal increases national coverage, scope of services, and market leadership as the largest, most comprehensive provider…
Reasons to be a Perfusionist in Salt Lake City
Have you ever dreamed of whisking away to live in one of the happiest cities in...Reasons to be a Perfusionist in Boca Raton
It really doesn’t get much better than Boca Raton, Florida. With tropical weather all year round...Be a Perfusionist in Palmdale, California
Palmdale, California. You may not have heard of it, but it’s practically a distant suburb of...What’s It Like to Be a Surgical Neurophysiologist in Colorado Springs?
If you’re a surgical neurophysiologist considering making Colorado Springs, CO, your home, there are a few...What’s It Like to Be a Surgical Neurophysiologist in San Francisco?
San Francisco, California, is a tourist destination and technology hub, boasting colorful neighborhoods and a thriving...From Personal Assistant to IONM Clinician, SpecialtyCare Associate Finds Her Calling
Happy Neurodiagnostic Week! I’m Martha Ross, an IONM clinician primarily working in Nashville, Tennessee. In just…
History of IONM
Intraoperative neuromonitoring (IONM), the consistent monitoring of a patient’s central nervous system during a surgical procedure,…
Perfusion Careers in Coatesville, Pennsylvania
SpecialtyCare is currently hiring for a perfusionist in Coatesville, Pennsylvania. If you’re certified and interested in...Perfusionists Needed in San Jose, California: Why You Should Consider a Move
San Jose, California. With 257 sunny days a year, stunning scenery and some of the friendliest...Vegas is Calling: It Needs Perfusionists!
In case you were wondering, the answer is yes. SpecialtyCare is currently hiring in Las Vegas....Ready for a Beach Move? Perfusionists Needed in Panama City, Florida!
Panama City, Florida. Chances are you’ve probably been there on vacation at some point in your...‘Obesity Paradox’ Doubtful for Blood Transfusion Risk
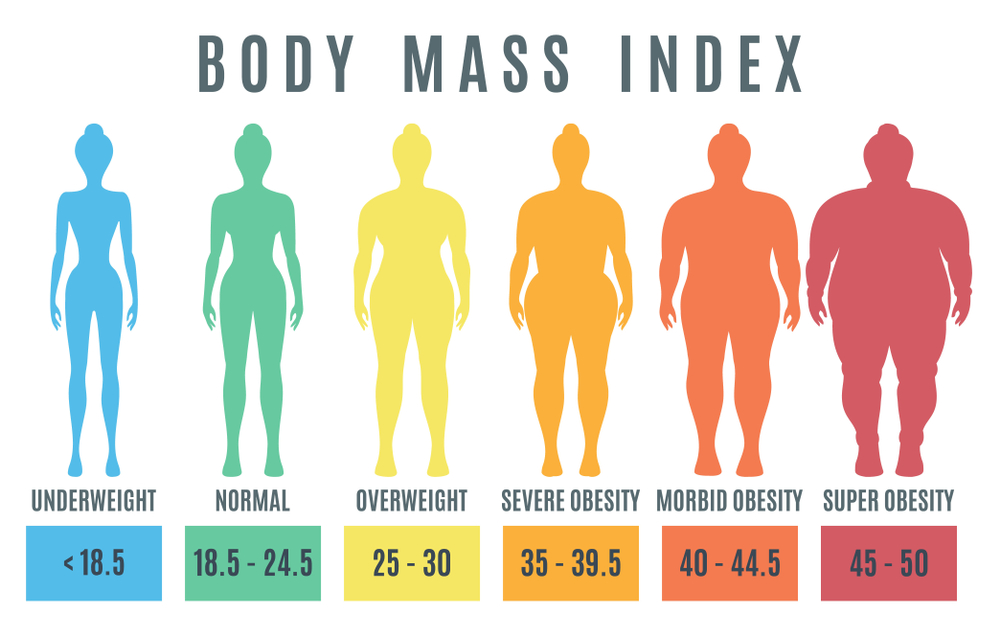
The study, “A BMI >35 does not protect patients undergoing cardiac bypass surgery from red blood…
Reasons to Consider a Perfusion Career in Wichita, Kansas
Wichita, Kansas. The big city with the small hometown feel. While it may be the biggest...Why You Should Be a Perfusionist in Kenosha, Wisconsin
Kenosha, Wisconsin. A beautiful small city right off Lake Michigan is tough to beat. With sandy...Being a Perfusionist in Reading, Pennsylvania: What are the Benefits?
Reading, Pennsylvania. Unless you’re a native of the state, chances are you’ve never heard of this...Work for SpecialtyCare in Milwaukee, Wisconsin
For those of you out there who are already in the IONM field and looking for...Looking for a New IONM Career? Experience Small-town Living in Dyer, Indiana
It wouldn’t be a big surprise if you’ve never heard of Dyer, Indiana. Most people haven’t....IONM Job Opportunities in Indianapolis, Indiana
Indianapolis, Indiana. Indy. Circle City. Crossroads of America. Whatever nickname you choose, the great American city...Reducing a Bypass Pump’s ‘Prime Volume’ a Good Practice—Up to a Point
Study findings, “The Unintended Consequences of Over-Reducing Cardiopulmonary Bypass Circuit Prime Volume,” were published in the…
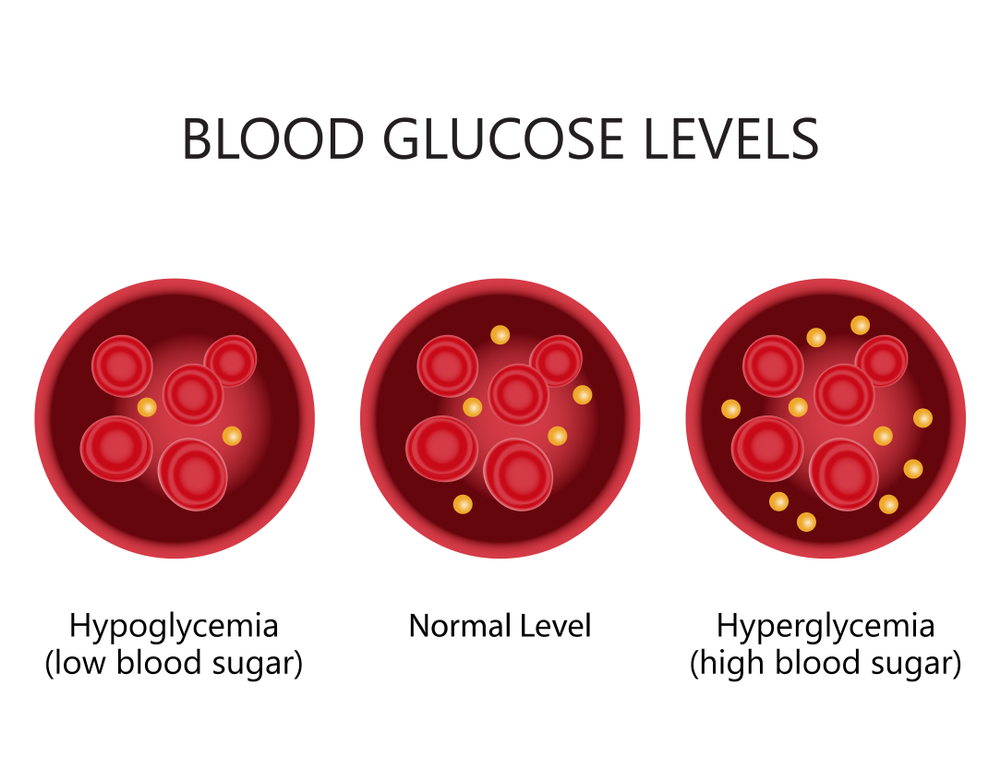
What Protects the Heart During Surgery Also Impacts Blood Sugar Levels
Review the study findings, “Does the Type of Cardioplegia Solution Affect Intraoperative Glucose Levels? A Propensity-Matched…
Work for SpecialtyCare in Green Bay, Wisconsin
For certified surgical neurophysiologists with at least 2 years of experience who are looking for something...Patients May Benefit From ‘Ultrafiltration’ of Their Blood During Cardiac Surgery
Review the published study, “The effect of ultrafiltration on end-cardiopulmonary bypass hematocrit during cardiac surgery,” published…
Perfusion Industry Leader SpecialtyCare Welcomes Kirti Patel
FOR IMMEDIATE RELEASE Contact: SpecialtyCare Lee Pepper, 615-345-5572 Chief Marketing Officer [email protected] Brentwood, TN, January 14,…
Working as a Perfusionist in Richmond, VA: What Are the Benefits?
Richmond, VA, is a city steadily growing in size and popularity, but its expansion has not...Working as a Perfusionist in Urbana, Illinois: What are the Benefits?
If you’ve been checking out this blog section, you’ve noticed by now that we’re closely examining...Working as a Perfusionist in Cumberland, Maryland: What are the Benefits?
SpecialtyCare is currently looking for perfusionists for our Cumberland, Maryland positions. Nestled near the Potomac River...Sonia Zuzek, Director of Clinical Education Featured on WSMV Channel 4
Sonia Zuzek, SpecialtyCare’s Director of Clinical Education, was featured on WSMV Channel 4. She discusses the…
Working as a Perfusionist in Somerset, Kentucky: What are the Benefits?
Somerset, Kentucky. If you’re a perfusionist and also a fan of the small town life, then...Working as a Perfusionist in Parkersburg, WV: What Are the Benefits?
Parkersburg, WV, is a city for those who enjoy the great outdoors and a quaint community...Working as a Perfusionist in Harrisburg, PA: What Are the Benefits?
Harrisburg, PA, offers many historical attractions and opportunities for outdoor recreation. The cost of living is...Reasons to Be a Perfusionist in Visalia, CA
As you may have already seen on sites like Glassdoor and Jobs.net, SpecialtyCare is growing at...Reasons to be a Perfusionist in Irvine, CA
Fun fact. You’ve probably seen glimpses of Irvine, California, before and didn’t even realize it. Nestled...Why You Should Be a Perfusionist in Palm Springs
Palm Springs, California. We’ve all seen glimpses of it on countless TV shows. A weekend getaway...Top 5 Most Interesting Perfusion Statistics
If you’ve spent some quality time on our site, you already know the perfusion field is…
Are You Growing in Your Career as a Perfusionist?
5 Questions to Ask about Your Current Job Situation With perfusion services in high demand at...What If I Can’t Afford Perfusion School?
Good news for those who want to enter the perfusion field: perfusionist schools/programs are relatively inexpensive…
The Perfusionist Path: From School to Salary
If you’ve found your way to this article, then chances are you are at least somewhat…
An ECMO Miracle
It was a warm Summer night in July. Courtney Novello, a clinical perfusionist (and now clinical…
Top Five Reasons to be a Perfusionist
We’ve talked a lot on our SpecialtyCare site about what it means to be a perfusionist....SpecialtyCare Addresses Perfusionist Shortage with Brown-Brukardt Scholarship
Each year, 350,000 people require open-heart surgery and related cardiovascular perfusion support. These procedures require a…
SpecialtyCare Awarded Ambulatory Health Care Reaccreditation From the Joint Commission
BRENTWOOD, TN – Nov. 28, 2018 – SpecialtyCare, the largest provider of outsourced intraoperative neuromonitoring (IONM) services,…
Special Gift Reminds Dr. Sam Weinstein of Time on the Navajo Nation
It has all the makings of a Hollywood script. A young doctor in between residencies packs…
Re-Certified by The Joint Commission
SpecialtyCare re-certified by The Joint Commission and scores 100% for their third consecutive audit. We are…
Perfusion Careers in Texas
There’s that old saying that everything is bigger in Texas. So is the need for perfusionists….
SpecialtyCare Sponsors Knights 5K@5
Registration funds will support athletics and special education at Nolensville High SpecialtyCare loves to give back…
SpecialtyCare Acquires Intraoperative Neuromonitoring Provider Precedent Health
NASHVILLE, Tenn.—SpecialtyCare—the nation’s leading provider of outsourced intraoperative neuromonitoring (IONM), perfusion, and surgical services—announced today that…
Jonathan Walters, President, Intraoperative Neuromonitoring at SpecialtyCare, on WSMV
Jonathan Walters, President, Intraoperative Neuromonitoring at SpecialtyCare, recently got a chance to sit down with WSMVTV…
Supply Drive Success!
SpecialtyCare staff participated in a back-to-school drive, supporting our partner nonprofit PENCIL and its free school…
Neuromonitoring with the Spinal Brigade in Honduras
The World Pediatric Project coordinates and mobilizes surgical, diagnostic, and medical specialty teams to provide treatment for young people in countries where advanced pediatric care is unavailable to children in need. I was lucky to be invited on a mission trip to Honduras as part of this program. It was an incredible experience, one that I will l never forget.
Moving Beyond Surgeon Preference: Consolidating IONM Providers
How much a hospital spends on surgical supplies and staffing depends largely on its physicians, who drive 75-85% of all quality and cost decisions. Much like the selection of surgical supplies, the choice of intraoperative neuromonitoring (IONM) providers has traditionally been left to the surgeons. As a result, it’s not uncommon to have three or more IONM providers supporting different surgeons within the same hospital. This often leads to unnecessary operational complexity and high managerial costs. And, while many non-consolidated, multi-provider environments originate from surgeon preference, they can actually have a negative impact on surgeon satisfaction. Consolidating providers is an attractive solution, but consolidation cannot be accomplished without surgeon buy-in, and that requires careful planning and coordination.
SpecialtyCare Names Recipients of 2018 Brown-Brukardt Perfusion Education Scholarship
SpecialtyCare’s education scholarship program is designed to support and assist cardiovascular perfusion students who demonstrate the potential to advance patient-focused care in a way that honors the legacies of Jim Brown and Gary Brukardt. The selection committee was delighted by the strong response and overwhelming quality of this year’s candidate pool, which further illustrates the extraordinary talent and commitment of our finalists. With this in mind, I am pleased to announce that the recipients of the 2018 Brown-Brukardt Perfusion Education Scholarships are Jacki Brolhorst and Robert DeGiosio. We are confident that they will make significant contributions to patients’ lives and the practice of cardiovascular perfusion for years to come.
SpecialtyCare is First IONM Provider to Gain ABRET Recognition
The ABRET Neurodiagnostic Credentialing and Accreditation Board has recognized SpecialtyCare’s Intraoperative Neuromonitoring (IONM) Training Program with formal Neurophysiologic Intraoperative Monitoring program status. This makes SpecialtyCare one of only two training programs, and the sole clinical services provider, to achieve this recognition. With approval as a recognized program, our surgical neurophysiology trainees gain Pathway IV eligibility for ABRET’s Certification in Neurophysiologic Intraoperative Neuromonitoring (CNIM) testing.
Hillsboro High Students Scrub Up at SpecialtyCare
PENCIL is a terrific organization that helps Metro Nashville Public School students achieve academic and future success. As a proud PENCIL Partner, SpecialtyCare regularly hosts students from Hillsboro High School’s Academy of Global Health & Science. Our fully equipped simulation operating room, or Sim OR, which is used to train our staff, provides the perfect environment to introduce the students to life as a member of a surgical team. Our Nashville IONM Operational Leadership and the IONM Education Team have designed an elite experience for the students to actively learn about electrophysiology and participate in a virtual surgical procedure that utilizes intraoperative neuromonitoring to assist the surgeon and keep the patient safe during surgery.
Significant Savings Shown in New Analysis of Intraoperative Autotransfusion
The risks and complications of blood transfusion are well documented. One technique commonly used to help reduce the need for bank blood is autotransfusion, also referred to as intraoperative autotransfusion (IAT) or autologous blood transfusion. IAT is a method of collecting the patient’s blood lost during surgery, processing it, and returning it to the patient. This can significantly reduce, or even eliminate the need for blood transfusions, which in turn reduces complications and the cost of care.
Apply for the 2018 Brown-Brukardt Perfusion Scholarship
SpecialtyCare’s Executive Leadership supports the funding of perfusion education tuition for two students enrolled in CAAHEP-accredited programs. We will begin accepting the next round of applications for the Brown-Brukardt Perfusion Scholarship Program on December 1, 2017. Perfusion is both a vital medical service and a smart career choice. About 350,000 people need open heart surgery and related cardiovascular perfusion support every year. However, hospitals are currently experiencing a perfusionist shortage, and qualified experts are in high demand. We are committed to actively recruiting smart, motivated men and women into the field to ensure that surgeons and patients have skilled perfusion care available when they need it most.
Credentialing: Gatekeepers to Patient Safety
When a person is under medical care, the patient and his loved ones need to trust that the practitioner is educated, licensed, and trained in the specialty. And that’s where medical staff professionals (MSPs) come in. We maintain credentialing and licensure information, implement federal rulings and accrediting standards, and enforce the rules, regulations, and policies that govern the activities of medical staff. More than 2,000 MSPs gathered recently for the 41st National Association Medical Staff Services Educational Conference & Exhibition in Colorado Springs. The event was the perfect run-up to National Medical Staff Services Awareness Week, so I’d like to offer a recap of the conference as we celebrate the team at SpecialtyCare, and their counterparts all across the country, who work hard behind the scenes to ensure patient health and safety.
Why Doesn’t Everyone Have a PBM Program?
On November 3rd, we were honored to accept the 2017 Delaware Valley Patient Safety & Quality Award from The Health Care Improvement Foundation for our submission, “Implementation of a Patient Blood Management Program,” which outlines the integration of patient blood management (PBM) as a daily, embedded quality improvement strategy at Thomas Jefferson University Hospitals (TJUH). The project was evaluated on evidence of significant and sustained improvement in quality, patient safety, innovation, and the potential for replication in other healthcare organizations. As an outsourced provider of PBM implementation, we are thrilled to share in TJUH’s success and we applaud its leadership and organizational commitment to improvement.
Answering the Call When Tragedy Strikes
In Puerto Rico—more than one month after Hurricane Maria devastated the island—many communities still lack the water, electricity, pharmaceuticals, communications, transportation, and other resources needed to sustain life and care for patients. At Hospital Español Auxilio Mutuo in San Juan, our cardiac perfusion team works under these challenging conditions to provide medical care, which has included a successful aortic dissection repair performed with the patient under deep hypothermic circulatory arrest while the hospital was on generator power.
OR Excellence Conference: Thinking Beyond Familiar Strategies
Mitigating risk is top of mind in healthcare right now. The OR Excellence Conference hit this topic and many more head-on during its 9th annual gathering in Las Vegas. With 400 OR professionals in attendance, the conference curriculum focused on hospitals improving clinical outcomes, expanding caseloads, growing more profitable, and protecting staff and assets, all in an innovative and interactive learning format. Attendees are constantly looking for ways to protect their patients, succeed economically, and position their hospitals for the future while mitigating the risk of moving away from volume-based reimbursement to value-based care tied specifically to improving patient outcomes and minimizing clinical variation.
The 30th Annual OR Manager Conference in Orlando: Turning Healthcare Uncertainty into Something Magical
The OR Manager Conference is the premier executive-level event for OR directors and OR business managers concerned with management of the surgical suite, and is dedicated to providing industry solutions and leading best practices. With 1,400 executive OR professionals in attendance, the focus this year was to improve efficiency and affectivity with sessions on patient safety, infection control, OR flow, staff motivation, and leadership. All of these topics were discussed in keynotes, in sessions, in networking events, and in the exhibit hall in the context of preparing strong OR leaders for the unpredictable climate we’re currently experiencing in healthcare.
SpecialtyCare OptimizeOR Takes the Guesswork Out of Perioperative Improvement
Data-driven, metric-based healthcare is required in today’s value-based environment and essential for sound decision-making. Without it, you’re simply guessing. Cost reductions and real increases in volume, efficiency, and ultimately revenue can be achieved when data and analytics are at your fingertips. That’s why we are excited to introduce SpecialtyCare OptimizeOR™, a user-friendly decision support and analytics system that helps OR managers improve productivity in perioperative performance. OptimizeOR software pulls your key performance measures into an easy-to-use online interface so that you can better manage resources for improved scheduling, staff allocation, and supply utilization. Optimized resource management makes space for increased case volume, minimizes inefficiency, reduces unnecessary spending, and drives patient and surgeon satisfaction.
SpecialtyCare and Perfusion.com to Present an Unparalleled Cardiac Perfusion Education Conference
When hosts of the two most prominent perfusion education conferences join forces to create a single premier event, you can count on a four-day learning experience like you’ve never attended before—and that’s what SpecialtyCare and Perfusion.com have planned in 2018. For 30 years, SpecialtyCare hosted Mechanisms of Perfusion, one of the industry’s most highly regarded advanced learning forums. The Sanibel Symposium, hosted by Perfusion.com, has also earned a reputation as an elite, highly attended meeting, both in person and via their live webcasts. So, we are thrilled to now combine our expertise and resources to present The 2018 Sanibel Symposium, an unparalleled cardiac perfusion learning event at the Sanibel Marriott Resort and Spa in Ft. Myers, Florida, April 4-7, 2018.
Patient Blood Management: Balancing Outcomes with the Cost of Healthcare
In healthcare, the sweet spot is the perfect balance of healthcare spending and patient outcomes. It’s the place of equilibrium that features just the right type and degree of patient care while avoiding the cost and potential harm of unnecessary interventions. Some providers have learned that balancing both clinical and economic concerns must begin on the most basic level—with a check of the patient’s blood health—and implementation of effective patient blood management (PBM) strategies.
Use of IONM During Cervical Spine Surgery Associated with Reduced Opioid Use, Readmissions
“We have an enormous problem that is often not beginning on street corners; it is starting in doctor’s offices and hospitals in every state in our nation.” This quote comes from the recent interim report by the Commission on Combating Drug Addiction and the Opioid Crisis. Since 1999, the number of opioid overdoses in the U.S. has quadrupled. Over that same period, the amount of prescription opioids sold has quadrupled as well. With a substantial portion of the population experiencing chronic pain and more than 650,000 prescriptions dispensed every day, the medical profession must employ every available strategy to address the tragic human and economic costs of opioid misuse, abuse, and dependence. One such tactic is to avoid the need for prescription opioids in the first place, or to limit a patient’s pain management need to a very short duration.
Prioritize Communication to Improve Clinical Performance
Communication in the OR is vital to patient health and safety. Late starts, delays and interruptions, decreased surgeon satisfaction, tension in the OR, and clinical errors often can be attributed to miscommunication or the lack of communication. The effect on patients can be devastating, resulting in readmission, a life-long chronic condition, or worse. The Joint Commission and other organizations routinely list communication failure as one of the most frequent causes of sentinel events, but many “never events” and other problems can be avoided with structured processes and an organizational commitment to prioritize communication.
Don’t Let an Iceberg Sink Your Clinical and Financial Outcomes
Parts of the United States are experiencing record-breaking heat this summer, and yet, icebergs are everywhere! Icebergs—the classic metaphor for situations wherein most of the substance (and risk) hide below the surface—have been used to discuss topics as varied as psychology, homelessness, big data, influence, safety, Hemingway, and school performance. Risks hidden below the surface are prevalent in healthcare, too. When teams assess their clinical outcomes, some factors are clear and measurable. These parts of the iceberg are above the surface, and hospitals increasingly are held accountable for them. Other outcomes, or factors that affect outcomes, are lurking within the complexity of hospital operations but are demonstrably significant in the future health of the patient.
More Hospitals Finding Value in Sterile Processing Consultants
Imagine you’re riding a bicycle that slips a chain. It’s a basic fix, but you have to stop pedaling to do it. When your sterile processing chain slips, you don’t get to stop, and it’s very difficult to fix the bike yourself while you’re still pedaling. Hospital administrators and managers focused on continuous improvement are increasing attention on their sterile processing departments to improve quality, efficiency, surgeon satisfaction, and patient care. An outside sterile processing consultant who has the expertise to conduct a useful assessment and create and implement strategic plans can quickly jump start a quality improvement program without disrupting the department’s regular activities. This is a significant advantage over an in-house approach to improvement. As a result, many leading hospitals are engaging expert consultants for help.
Surgical Neurophysiologist Graduates Continue Certification Streak
The evolution from a wide-eyed trainee to a professional surgical neurophysiologist capable of supporting surgeons in the most complex procedures is a metamorphosis that is truly awesome and, with every graduating class, I’m reminded of the tremendous group effort behind the scenes. Our clinical instructors, medical office staff, senior surgical neurophysiologists, remote monitoring professionals, and operations leaders provide support and guidance every step of the way. This spirit of teamwork not only makes the training program successful, it also makes the goals of clinical excellence, continuous improvement, and patient-centered care achievable. I am thrilled to be part of such a group and I cannot wait to see our newest team members grow into the next SpecialtyCare IONM mentors and leaders.
One Compliance Violation Headline is One Too Many
Illegal referrals and inaccurate billing are often inadvertent, but can be part of deliberate and deceptive moneymaking schemes when physicians and other clinicians have ownership in outsourced providers for hospitals. Whether intentional or not, there is an ongoing pattern of regulatory compliance violations relating to the False Claims Act, the Stark Law, and the Anti-Kickback Statute. Headlines continue to regularly highlight fraudulent billing and illegal referrals that pose tremendous risk to hospitals, providers, and patients. Even alleged violations and pre-trial indictments can be costly given that regulatory agencies are authorized to suspend federal payments to providers under investigation.
SpecialtyCare IONM Mission Trip to Moldova
In the fall of 2016, David Citarrella, SpecialtyCare’s Director of Operations for Intraoperative Neuromonitoring (IONM) in California and Nevada, let me know that an orthopedic surgeon in San Francisco planned to travel to the Republic of Moldova in Eastern Europe on a humanitarian mission. The surgeon, Dr. Dimitriy Kondrashov, had inquired about the use of IONM equipment to monitor spinal procedures during his trip. My first thought was, “What is he going to do with this equipment? It’s not like you just press one button to turn it on, then get a green light if all is good, or a red light if there is a problem.” I reached out directly to Dr. Kondrashov to see if I could help.
New Research on Alerts and Postoperative Deficits from the ACNS Annual Meeting
Scientists have been fascinated with the workings of the human nervous system dating back to the time of Hippocrates and well before. Today, as members of the healthcare community gain a greater understanding of the system—how to treat its disorders and protect its integrity—interest in the topic continues to grow. The American Clinical Neurophysiology Society (ACNS) has been a leader in education and training for the past 70 years, and its recent annual meeting continued this tradition. SpecialtyCare was pleased to present two new research studies at the event to advance the community’s understanding of intraoperative neuromonitoring (IONM) and its impact on patient health and safety.
Celebrating 40 Years of Advancements in Neuromonitoring
The American Society of Neurophysiological Monitoring (ASNM) is “dedicated to the advancement of quality neurophysiologic monitoring services for neuroprotection.” Stated more simply, it’s all about patient safety. SpecialtyCare is deeply committed to supporting the Society and its mission to grow the profession, provide educational forums, develop quality standards, and build partnerships with allied healthcare professionals. As part of this commitment, members of our team serve in leadership roles with the ASNM and recently contributed several presentations at the organization’s Annual Meeting in May, an event celebrating 40 years of neuromonitoring.
Intraoperative Autotransfusion: A Key Blood Management Strategy
Evidence-based patient blood management (PBM) strategies offer significant clinical benefits. Conservation techniques, in particular, help minimize the use of allogeneic red blood cell transfusion, which has been shown to increase the risk of postoperative complications, readmissions, and mortality among patients. Because of the importance of this area of study, SpecialtyCare researchers continue to drill down and analyze the perfusion and autotransfusion cases in SCOPE, the SpecialtyCare Operative Procedural Registry™, to examine the impact of various strategies, develop best practices, and improve patient outcomes.
SpecialtyCare Cardioplegia Research Presented at AmSECT – AATS Meeting
To strengthen alignment among multiple surgical disciplines, the American Society of ExtraCorporeal Technology (AmSECT) and the American Association for Thoracic Surgery (AATS) teamed up to present a terrific joint learning opportunity, holding AmSECT’s 55th International Conference in conjunction with the Centennial Meeting of the AATS in Boston. The integrated program was designed to improve care by bringing surgeons, perfusionists, and other experts together to foster effective communication and coordination in the operating room. The combined meeting was a great example of collaboration that advances quality through evidence-based learning and improvement. We are proud to have been part of this special event.
Patient Blood Management Aligns with Value-Based Healthcare Goals
Both the American Medical Association and The Joint Commission consider red blood cell transfusion to be among the five most overused procedures, yet it remains one of the most commonly performed medical interventions in U.S. hospitals today. Vague clinical guidelines and long-held norms have created wide variation in the use of transfusion, but many administrators and clinicians are now realizing that reducing transfusion rates with evidence-based patient blood management programs can provide significant clinical and economic benefits.
How Surgical Assistants and Surgeon Satisfaction Collide
It’s hard to overstate the importance of trust and confidence in the operating room when so much is on the line. The surgeon needs to know that every member of the OR team is experienced and reliable. This is especially true of the surgical assistant, who serves as an extension of the physician before, during, and after the procedure. In addition to providing exceptional clinical skills, a valuable surgical assistant (SA) understands the surgeon’s preferences and enables a rhythm and a shorthand that promote successful patient outcomes and surgeon satisfaction.
Mothers Inspire Us at Home and in Careers
This weekend is Mother’s Day. The women who nurtured our young selves also inspired us to dream of who we could become. Many of us grew up witnessing these special women diligently pursuing excellence in scientific or health-related careers, and we chose to follow similar paths. Here are a few tributes to the mothers behind our SpecialtyCare family. We encourage you to take a few minutes to remember the women whose love and inspiration made a difference in your life.
Six Questions for Targeting a Minimally Invasive Partner
In the original Star Wars movie, we cheered as the Rebel Alliance strike teams zipped through the trenches of the Death Star to hit a tiny target and win a great victory. (Yes, today is Star Wars Day – May the Fourth be with you!) Laparoscopic surgeons use similar tactics as they navigate narrow openings in tightly focused procedures to help patients achieve big improvements. As demand for such services continues to increase and your hospital grows its laparoscopic services, you’ll need a minimally invasive surgical support (MISS) program you can rely on. Our latest guide, The True Value of a Minimally Invasive Partner in Your OR, will help you navigate the process of providing a strong, integrated partner for your surgeons and OR teams.
Engage Your Surgeons for Performance Improvement
Sometimes a few fundamental changes can breathe new life into an existing process and, as a result, enhance the performance of your surgeons and staff. Even if your routine is working relatively well, service line changes in your operating room can achieve improved results, such as higher levels of surgeon satisfaction and patient care quality, both of which can generate greater value for your organization and your patients. But any changes in and around the surgical suite need surgeon support to optimize success. Here are six guidelines to help engage surgeons as a first step toward project planning and improved performance.
Evaluating the Real Cost and Value of Your Perfusion Services
Perfusion is an integral part of your hospital’s cardiovascular care program, but the overhead costs and administrative burden of maintaining and managing a team of reliable perfusionists with advanced skills can pose challenges for program administrators. It can be easy, however, to overlook both the indirect costs and benefits of clinical services. So, whether your perfusion is handled in-house or outsourced, we’ve developed a new guide, The Real Spend of Your Perfusion Program: Twelve Tips to Discover the True Value, to help you evaluate your program and any changes that you might be considering.
AORN 2017: A Continuing Commitment to Quality Care
AORN 2017 was the place to be for perioperative registered nurses and others who share a continuing commitment to quality care. Nurses, and the hospitals they represent, are constantly looking for ways to improve patient outcomes while also reducing the cost of care. Both of these goals were addressed in some of the most talked-about educational sessions and posters presented during the conference. Cost containment and better clinical outcomes were also recurring themes among the 600 attendees who visited our booth. In addition to exhibiting, we hosted an educational networking dinner that featured a presentation on one of healthcare’s hottest topics—patient blood management (PBM).
Do You Know the Real Cost and Value of Your IONM Provider?
We all want the best quality for the best value, but it’s often difficult to evaluate our options accordingly. Hospitals that are exploring outsourced intraoperative neuromonitoring (IONM) options obviously want to know what they’re paying, which can be difficult when different vendors present different pricing models and different services. It can be like comparing apples to oranges to strawberries. They’re all fruit, but clearly not the same. Here are some quick tips for evaluating outsourced IONM services, taken from our new guide, The Real Spend of Your IONM Program: Eight Tips to Discover the True Value.
Women in STEM Education: Developing Future Healthcare Leaders
We hear a lot these days about STEM education—an interdisciplinary, applied approach to teaching science, technology, engineering, and mathematics. The rise of women in STEM careers is notable, too. So, as Women’s History Month draws to a close, we decided to look to the future being built right now by some of the women at SpecialtyCare who pursued careers in science and are responsible for our clinical education and training programs today. Each has had a unique journey that includes education, choices, gumption, and surprises. They actively honed their interests and cultivated their talents to reach their current roles, and they continue to apply their strengths toward additional growth for themselves and others—men and women alike.
PENCIL Partnership Introduces High School Students to Healthcare Careers
In 1982, PENCIL Foundation—an alliance of business leaders and local school administrators—was created to provide new opportunities that promote achievement by young people enrolled in Nashville’s metro public schools. The Foundation’s PENCIL Partners program now includes more than 800 community-school partnerships that serve over 80,000 students. As a proud member of PENCIL Partners, SpecialtyCare regularly hosts students from Hillsboro High School’s Academy of Global Health & Science to introduce them to careers in the healthcare field.
No Debate Needed: Compliance Violations Increase Healthcare Costs
A complex system offers a lot of places to hide bad behavior. Medicare and Medicaid—programs at the heart of the current healthcare debate—are particularly vulnerable to violations of Stark Law, the Anti-Kickback Statute, and the False Claims Act. Nearly every day, the Office of Inspector General (OIG) issues details of individuals and hospitals being charged or convicted of healthcare fraud and abuse. Financial penalties and the possibility of imprisonment aside, damning headlines can destroy the bottom line and reputation of even the most respected providers. Compliance violations drive up healthcare costs and compromise patients who are overcharged or subjected to unnecessary tests and treatments.
Consolidation Contributes to Delivery of Higher Value Care
Consolidation in healthcare is nothing new, in fact it’s hotter than ever. Most analysts, and others who know the industry well, will tell you this trend is positive as we seek better patient outcomes, operational efficiencies, and cost containment to deliver higher value care. In the outsourced medical service provider sector of healthcare, we also can increase value with mergers and acquisitions. As the sector matures, consolidation offers new opportunities to provide customers with high quality, specialized, and reliable services that support hospitals’ goals within today’s rapidly changing healthcare environment.
The Effect of Ultrafiltration on End-Cardiopulmonary Bypass Hematocrit during Cardiac Surgery
Collaborating and sharing research findings and best practices with other medical professionals is one of the great pleasures of working in healthcare. Recently, the American Academy of Cardiovascular Perfusion’s 38th International Meeting gave SpecialtyCare’s Medical Office team members the opportunity to present two new papers to the perfusion community. One of the studies examines “The Effect of Ultrafiltration on End-Cardiopulmonary Bypass Hematocrit during Cardiac Surgery.” The purpose of this research was to evaluate the effect of ultrafiltration on end-cardiopulmonary bypass hematocrit by cardiac surgical procedure type. The findings are summarized in today’s blog.
Congratulations to Our Brown-Brukardt Perfusion Scholarship Recipients
When we decided to create the Brown-Brukardt Perfusion Scholarships program in honor of Jim Brown and Gary Brukardt—men who helped advance the practice of perfusion—we felt it was important to find and support students with the potential to drive improvement in healthcare like Jim and Gary did throughout their careers. Today, we are proud to announce that Cassandra Wuest and Kyle Zelesnick are the recipients of our 2017 perfusion education scholarships, and they are even more talented and impressive than we had hoped.
AACP 2017 Best Paper: The Effectiveness of ANH and AP on Blood Management
Recently I attended the 2017 Annual Meeting of The American Academy of Cardiovascular Perfusion. The AACP, as always, offered strong educational content and a great opportunity to meet up with friends and colleagues. While there, I had the pleasure of presenting co-authored research on “The Effectiveness of Acute Normovolemic Hemodilution and Autologous Prime on Intraoperative Blood Management during Cardiac Surgery.” The AACP honored our team, which includes our perfusion associates and their tireless dedication to clinical excellence and data collection, by selecting this work as the meeting’s Best Paper. I encourage you to read the abstract for additional detail, but here’s a summary of our findings, which highlight the value of thoughtful perfusion strategies that can reduce the need for costly transfusions and increase the likelihood of better clinical outcomes.
A Few Simple Facts about New Reimbursement Models
Changes in reimbursement models are driving changes in operations, including data collection and reporting. Providers are being encouraged and incentivized to implement value-based care (VBC) that emphasizes cost savings and quality outcomes instead of the traditional fee-for-service (FFS) reimbursement model that pays according to the number of procedures performed. The idea is that when hospitals have financial incentives to be accountable for patient outcomes, then the comprehensive focus on quality will result in overall lower costs. Transitioning from FFS to VBC may be especially difficult for ORs with their high costs of procedures, but several strategies can help clear the path to progress.
Welcoming the People and Perfusion Expertise of Trident
SpecialtyCare has completed an asset purchase of Trident Health Resources, Inc., a highly regarded, clinically focused perfusion company. With the people of Trident joining SpecialtyCare and moving forward as one team, under one name, we have the opportunity to support each other and learn from each other as we participate in some of the most complex and interesting procedures performed today. We are uniquely positioned to define what superior clinical and financial outcomes look like and to provide those outcomes for our patients and our customers. We are thrilled to join together to serve as a resource for perfusion care and best practices that in-house and competitive programs simply cannot match. It’s an exciting time, and we look forward to all that we will accomplish together.
The Influence of Ultrafiltration on RBC Transfusion during CPB
Ultrafiltration is thought to reduce morbidity and the risk of red blood cell transfusion, however very few studies have examined the relationship between ultrafiltration and the overall risk of intraoperative RBC transfusion. Using data from the SpecialtyCare Operative Procedural Registry (SCOPE™), our study looks at a population of nearly 98,000 adults undergoing cardiac surgery at 197 hospitals to evaluate the effects of ultrafiltration volume removed during CPB on the relative risk of receiving an intraoperative RBC transfusion. Recognizing the findings of our own previous work, we were especially interested in testing potential differences between male and female patients in the effects of ultrafiltration.
Conquering Complexity: An MISS Implementation
Those of us who work in healthcare understand the importance of structured processes and clear communication during a patient handoff. Discontinuity puts the patient at risk and increases the likelihood of medical errors. As an outsourced OR services provider, a handoff takes on another meaning for us at SpecialtyCare—the transfer of an entire service without interrupting hospital operations or compromising patient care.
Live Every Day Like it’s Joint Commission Audit Day
The mission of The Joint Commission (TJC) is “to continuously improve health care for the public, in collaboration with other stakeholders, by evaluating health care organizations and inspiring them to excel in providing safe and effective care of the highest quality and value.” It’s a lofty goal, and one that has helped thousands of healthcare organizations improve. Unfortunately, the prospect of a TJC review is stressful and overwhelming for many healthcare providers. It doesn’t have to be. Check out these three things we’ve learned by designing and implementing a tested program that ensures that the people of our organization are always prepared to pass a stringent TJC evaluation while also meeting the requirements of our own internal quality programs.
Creating Certainty in an Uncertain Environment
From a healthcare perspective, the only thing we can be certain of in 2017 is that there will be uncertainty. For healthcare administrators, there is uncertainty around how to manage changes in provisions of the Affordable Care Act, Bundled Payments for Care Improvement (BPCI), and the Medicare Access and CHIP Reauthorization Act (MACRA). Restructuring Medicare and Medicaid could have a significant impact on planning, implementation, and payments for providers. But, regardless of the new format, healthcare providers like SpecialtyCare will always have an obligation—both to their patients and their customers—to improve value by providing high-quality care while containing costs.
Gender Differences in Intraoperative Blood Transfusions
It is a fairly well-known fact in the cardiac community that women have higher morbidity and mortality associated with coronary artery bypass (CABG) procedures. The reasons traditionally given for this disparity include women’s relatively smaller vasculature, higher incidence of anemia, and smaller circulating blood volume. Early in 2016, we in the Medical Department were discussing this phenomenon and decided to design a study using the robust data from our SpecialtyCare Operative Procedural Registry to find something in the intraoperative space that might be leading to these very different post-operative outcomes for men and women. Our findings were somewhat surprising.
Apply Now for SpecialtyCare’s Brown-Brukardt Perfusion Scholarship
SpecialtyCare is determined to drive awareness of perfusion as both a vital medical service and a smart career choice. As part of this effort, we are proud to officially launch the Brown-Brukardt Perfusion Scholarship Program. Every year, SpecialtyCare will award perfusion education tuition to two students enrolled in CAAHEP-accredited programs. Jim Brown and Gary Brukardt—men with close ties to SpecialtyCare who helped evolve the practice of perfusion over the last three decades—exemplified integrity, leadership, and dedication to patient care. Our goal is to support students who share these qualities and demonstrate outstanding potential as cardiovascular perfusionists.
Celebrating Behind-the-Scenes Contributions to Patient Care and Safety
It’s been said that “Everyone has a special talent, some are just flashier than others.” And so it is in healthcare. Behind every high-visibility physician and hands-on surgical team, there is a large group of people in back offices providing invaluable support. Everyone plays an important role—from human resources and training to accounting and scheduling. But today, as part of National Medical Staff Services Awareness Week, we proudly recognize our credentialing team at SpecialtyCare, and indeed in healthcare settings everywhere, for their contributions to quality patient care and safety.
NASS 2016 Best Paper: Neurologic Outcome Following Signal Change in Spine Surgery
The role of an expert IONM team is critical in the timely identification of adverse neurophysiologic changes and in promoting corrective action by the surgeon and anesthesiologist. Our research is based on clinical IONM data from SpecialtyCare’s Operative Procedural Registry. Taking advantage of big data—nearly 70,000 cases in this study—ensures that our conclusions are statistically significant, a vital aspect of evidence-based improvement in healthcare. It was an honor to present this study to such a prestigious group of surgeons at NASS and, in doing so, provide actionable information to help elevate the quality of care across the country.
SpecialtyCare Welcomes the People of Sentient to Our Team
On October 26, 2016, SpecialtyCare acquired Sentient, a highly regarded intraoperative neuromonitoring provider. We’re thrilled to welcome the people of Sentient to our team. We believe we’ll be a great fit together, both clinically and culturally. Combining our talent and experience will enhance our collective strengths and create new opportunities to advance patient care and drive clinical quality, which reduce costs for our patients and customers.
Teamwork Delivers Relief to Flood Victims
In August, a prolonged “no-name” storm deluged Louisiana, producing three times more rain than Hurricane Katrina. Lives were lost and the unprecedented flooding damaged or destroyed more than 100,000 homes and displaced thousands of people. As medical professionals, SpecialtyCare’s clinicians routinely step up when disaster strikes—we live and work in the communities we serve. But, stepping up can take different forms. In this week’s blog, we share a letter from a member of our intraoperative neuromonitoring group, who rallied the team to help the people of Louisiana.
You Think Your Job Is Tough? Imagine Being Sylvia Burwell
Sylvia Burwell, Secretary of the Department of Health and Human Services (HHS), is tasked with transforming our healthcare system from a fee-for-service model to a value-based system driven by the goals of access, affordability, and quality. Initiatives and legislation linked to Medicare, Medicaid, and other programs, such as the Health Insurance Marketplace and the Patient Protection and Affordable Care Act, have all but upended our healthcare system, sending providers, payers, and patients scrambling to understand and manage the changes.
One Man, Two Meaningful and Impressive Careers
When Richard Lawson talks with young people about their future, he sometimes suggests a stint in the military. Other times he suggests a career in the medical field. And sometimes, he suggests both. These are not just casual recommendations—he speaks from experience. Technical Sergeant Lawson is a military veteran and a member of the Kentucky Air National Guard. He is also a SpecialtyCare perfusionist. His discipline and dedication over the years has resulted in not just one, but two, meaningful and impressive careers.
Healthcare Fraud Is Not a Victimless Crime
Estimates vary when calculating the money lost to fraud—it’s difficult to measure that which is undetected—but the Federal Bureau of Investigation (FBI) states that healthcare fraud costs the country tens of billions of dollars each year. Paying for law enforcement, legal resources, and sophisticated technology to combat the problem adds to the price tag. Taxpayers and employers endure the financial brunt of fraud, but illegal schemes can also put patient health at risk. Clearly, healthcare fraud is not a victimless crime.
Surgeon Satisfaction: Small Adjustments Can Make a Big Difference
It’s not surprising that surgeons report high levels of burnout and a lack of professional satisfaction; nor is it surprising that the problem is getting worse. This creates concern for both the well-being of surgeons and the quality of patient care. As with other problems that might seem overwhelming, however, small adjustments can make a big difference. Here are some ways you can move the needle on surgeon satisfaction and, by extension, create efficiencies, lower costs, and realize better patient outcomes.
Spine Surgery Research: Alerts, Intraoperative Resolution, and Post-Op Deficits
Our intraoperative neuromonitoring (IONM) research studies show that IONM helps keep patients safe during surgery, decreases complications, and reduces costs associated with the use of analgesics, length of hospital stay, neurorehabilitation, and long-term chronic care. One such study, Neurologic Outcomes Following Differential Resolution of Neuromonitoring Alerts during Extradural Spine Surgery, examines the relationship between reversal of intraoperative neurophysiologic change and neurologic outcome following segmental spine surgery.
Replenishing Reserves: Engaging the Passionate Healthcare Professional
Building a highly talented clinical workforce is imperative for providing the best possible patient outcomes. We know, however, that the most passionate and effective healthcare professionals offer much more than clinical competence and they look for value in their work that extends beyond excellence in clinical care. They look for the intangibles and meaningful connections that prompted them to choose healthcare as a profession in the first place. Our goal is to sustain a culture where our people can thrive and find satisfaction, both personally and professionally.
Tracking and Tackling the Nontuberculous Mycobacteria Outbreak
The source of nosocomial infections can be elusive. For investigators, infections stemming from slow-growing bacteria are particularly difficult to identify and combat when symptoms do not present for months, or sometimes even years, after exposure. Add to these challenges the severity of potentially deadly infections and a bacterial outbreak can have devastating consequences. Such is the case with nontuberculous mycobacteria (NTM).
Improving Your Sterile Processing Department Starts with Focusing on the Fundamentals
Excellence in sterile processing management is fundamental to a well-run operating room. It supports on-time starts, surgeon satisfaction, and overall efficiency—all of which translate to financial results. But, most importantly, effective sterile processing management reduces the occurrence of healthcare-acquired infections (HAIs), which can significantly harm the patients entrusted to your care.
Goal-Directed Perfusion Methodology for Determining Oxygenator Performance During Clinical CPB
At the 37th Annual Meeting of the American Academy of Cardiovascular Perfusion (AACP), we presented research that used goal-directed perfusion methodology to determine oxygenator performance during clinical cardiopulmonary bypass. The study evaluates three oxygenators currently in clinical use and reflects how information collected by perfusionists could be utilized to provide new information to bridge gaps in knowledge when an absence of quality data is encountered.
The Obesity Paradox, Heart Surgery, and Blood Transfusion
Historically, there has not been a great understanding about the “obesity paradox,” which suggests that overweight and obese patients may have better outcomes than normal weight patients. Our newly published research confirms that while overweight and mildly obese patients do experience less blood transfusion and post-surgical bleeding than patients of normal weight, much of the observed reduction in transfusion rates in obese patients can be accounted for by other known confounds.
Best Practices in Team Collaboration and Infection Control
When I learned of a concern regarding Nontuberculous Mycobacteria (NTM) infections from use of LivaNova’s (previously Sorin) 3T heater-coolers and a change in their Instructions for Use (IFUs), I brought it to the attention of my OR Director at Memorial Medical Center. The situation has led to the development of best practices in team collaboration and infection control.
It Doesn’t Make Sense for Me to Replace My Own Roof
There’s good reason why I don’t roof my own house or fly my own plane. I rely on others for their specialized skills, experience, and economies of scale—knowledgeable people focused on specific activities that ensure quality and safety, keep costs in check, and know the codes and regulations that must be followed. Today, more than ever, we rely on specialization to get things done. Healthcare is no different. In fact, healthcare may be one of our best examples of an industry that can benefit significantly from specialized teams.
We Are Running Out of Perfusionists. And That’s A Problem We Need to Address
One of the most significant trends facing our industry today is the severe shortage of perfusionists. A current sample of 10% of active perfusionists found that nearly 50% are over 50 years old, and in 2015 there were almost 30% fewer new graduates entering the field than professionals leaving the field. This rate of decline cannot be sustained for long before the deficit poses serious risks to the 350,000 patients who need heart surgeries and perfusion services each year.